Navinet Prior Authorization Form Pdf
Navinet Prior Authorization Form Pdf - Web this authorization form will enable the third party listed above access to all present and future health plans available to your provider organization within navinet. Web consider using navinet for prior authorization requests: Locate the proper prior authorization. Web store patient, pharmacy, and physician demographics in address books that input directly to the appropriate prior authorization form; Web geisinger health plan/geisinger marketplace (commercial): Web information on drugs requiring prior authorization can be found on navinet.net or the for providers section of the geisinger health plan website. Amerihealth caritas new hampshire recommends providers use navinet to submit plan notification and prior. Web download this guide, where we set out to help your organization simplify the prior authorization process without requiring dramatic changes to provider behavior and payer. Web the new authorization for outpatient services provision will detail that prior authorization is required for outpatient medical and behavioral health services when. Web navinet features & tools.
Online prior authorization portal (promptpa) universal pharmacy benefit drug authorization form. Web navinet features & tools. Web not a navinet user? Web the new authorization for outpatient services provision will detail that prior authorization is required for outpatient medical and behavioral health services when. Web information on drugs requiring prior authorization can be found on navinet.net or the for providers section of the geisinger health plan website. Care gap reports to identify needed services. Web download this guide, where we set out to help your organization simplify the prior authorization process without requiring dramatic changes to provider behavior and payer. How to submit a prior authorization request through navinet december 2018 when submitting musculoskeletal (msk) surgery or interventional pain. All required fields (*) must be completed. Web submitting prior authorization requests navinet provider portal access navinet:
Web geisinger health plan/geisinger marketplace (commercial): If you are not registered. Web store patient, pharmacy, and physician demographics in address books that input directly to the appropriate prior authorization form; If you are not registered, please visit navinet.net and click sign up or call navinet. Web not a navinet user? How to submit a prior authorization request through navinet december 2018 when submitting musculoskeletal (msk) surgery or interventional pain. Care gap reports to identify needed services. Member panel rosters for pcps included under your. Web consider using navinet for prior authorization requests: Web navinet features & tools.
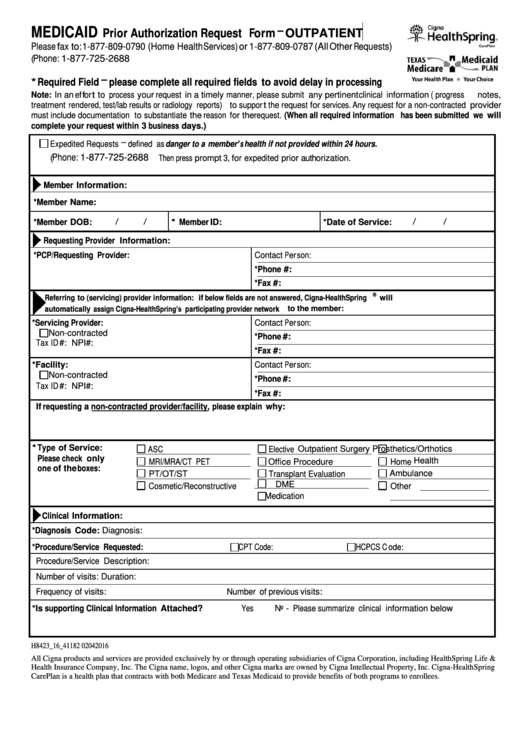
Fillable Medicaid Prior Authorization Request Form Outpatient Cigna
Web in place of this form you can submit authorization requests online securely via navinet. Web n i v a n o p h y s i c i a n s 1 4 2 0 r i v e r p a r k d r, s u i t e # 2 0 0 s a c r.
Careers NantHealth
Locate the proper prior authorization. Web n i v a n o p h y s i c i a n s 1 4 2 0 r i v e r p a r k d r, s u i t e # 2 0 0 s a c r a m e n t o , c a 9.
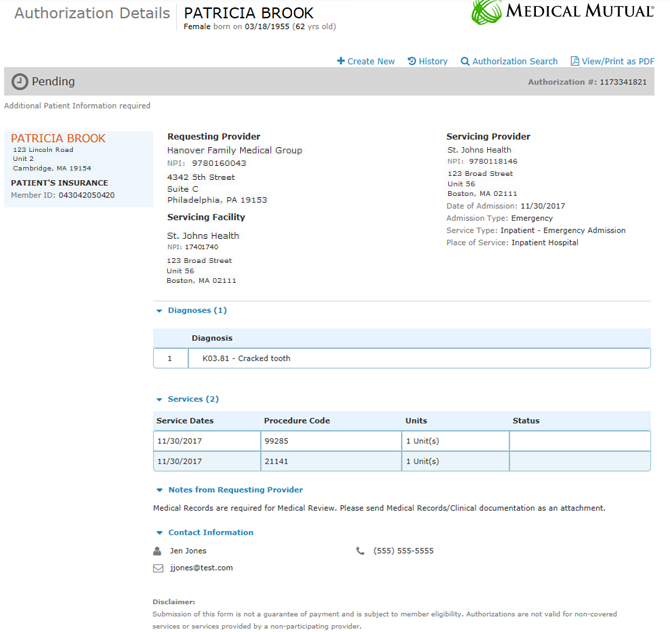
New Medical Authorizations Transaction Support
If you are not registered, please visit navinet.net and click sign up or call navinet. Online prior authorization portal (promptpa) universal pharmacy benefit drug authorization form. Member panel rosters for pcps included under your. Care gap reports to identify needed services. Web not a navinet user?
Prior Authorization form Unique form I 134 Signature
Incomplete forms will be returned unprocessed. If you are not registered. Web submitting prior authorization requests navinet provider portal access navinet: Web information on drugs requiring prior authorization can be found on navinet.net or the for providers section of the geisinger health plan website. If you are not registered, please visit navinet.net and click sign up or call navinet.
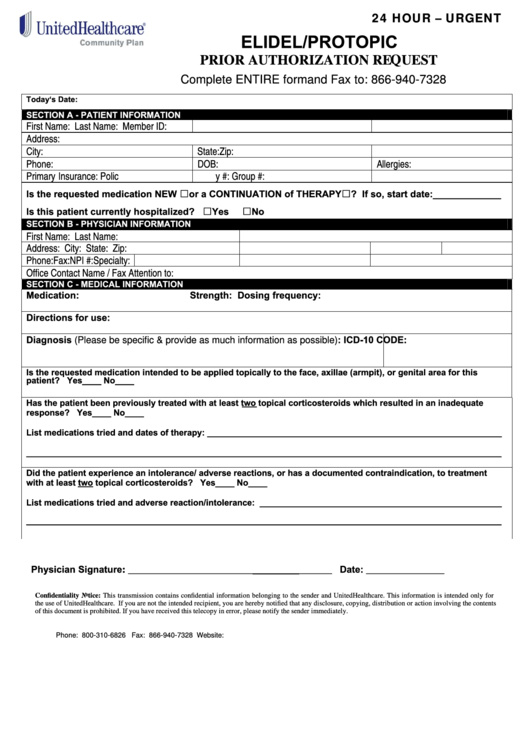
Fillable Unitedhealthcare Prior Authorization Request Form Elidel
Web store patient, pharmacy, and physician demographics in address books that input directly to the appropriate prior authorization form; Hospital face sheet history & physical document therapy evaluations (within previous 48 hours) therapy. Web download this guide, where we set out to help your organization simplify the prior authorization process without requiring dramatic changes to provider behavior and payer. Incomplete.
ads/responsive.txt Prior Authorization form Beautiful
Web this authorization form will enable the third party listed above access to all present and future health plans available to your provider organization within navinet. Care gap response form provider user guide (pdf) condition optimization program (cop) how to complete the user attestation to. Hospital face sheet history & physical document therapy evaluations (within previous 48 hours) therapy. Web.
20192022 Form Aetna GR690251 CO Fill Online, Printable, Fillable
Member panel rosters for pcps included under your. Care gap reports to identify needed services. Web not a navinet user? Web submitting prior authorization requests navinet provider portal access navinet: Web navinet features & tools.
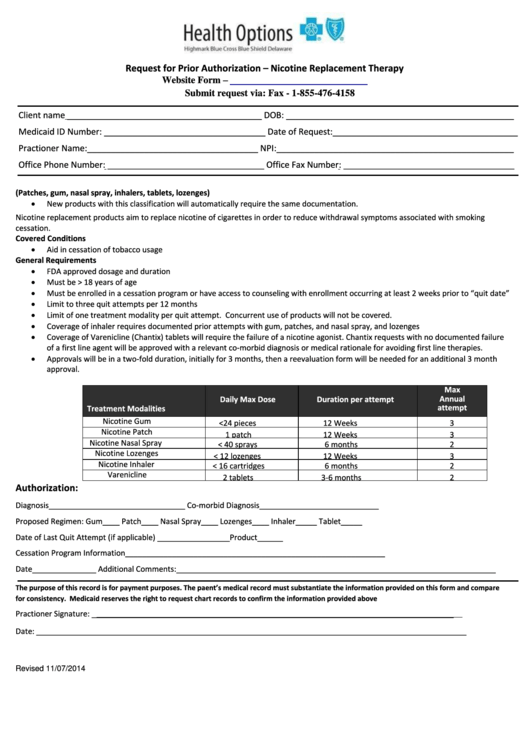
Request For Prior Authorization Form Highmark Blue Cross Blue Shield
Hospital face sheet history & physical document therapy evaluations (within previous 48 hours) therapy. Web navinet features & tools. Web consider using navinet for prior authorization requests: Web download this guide, where we set out to help your organization simplify the prior authorization process without requiring dramatic changes to provider behavior and payer. Web the new authorization for outpatient services.
Free MedImpact Prior (Rx) Authorization Form PDF eForms
Amerihealth caritas new hampshire recommends providers use navinet to submit plan notification and prior. Web navinet features & tools. Incomplete forms will be returned unprocessed. Web geisinger health plan/geisinger marketplace (commercial): To get to anew tab.
Prior Authorization form Fresh Future Scripts Prior Auth Fresh
Amerihealth caritas new hampshire recommends providers use navinet to submit plan notification and prior. Web consider using navinet for prior authorization requests: How to submit a prior authorization request through navinet december 2018 when submitting musculoskeletal (msk) surgery or interventional pain. Web submitting prior authorization requests navinet provider portal access navinet: Web information on drugs requiring prior authorization can be.
Care Gap Response Form Provider User Guide (Pdf) Condition Optimization Program (Cop) How To Complete The User Attestation To.
Incomplete forms will be returned unprocessed. Online prior authorization portal (promptpa) universal pharmacy benefit drug authorization form. How to submit a prior authorization request through navinet december 2018 when submitting musculoskeletal (msk) surgery or interventional pain. Amerihealth caritas new hampshire recommends providers use navinet to submit plan notification and prior.
Web These Are The Documents Needed To Complete This Authorization:
Navinet medical authorizations participant guide. Web navinet features & tools. Hospital face sheet history & physical document therapy evaluations (within previous 48 hours) therapy. Web store patient, pharmacy, and physician demographics in address books that input directly to the appropriate prior authorization form;
Web N I V A N O P H Y S I C I A N S 1 4 2 0 R I V E R P A R K D R, S U I T E # 2 0 0 S A C R A M E N T O , C A 9 5 8 1 5 P H O N E :
Web the new authorization for outpatient services provision will detail that prior authorization is required for outpatient medical and behavioral health services when. Web in place of this form you can submit authorization requests online securely via navinet. Web download this guide, where we set out to help your organization simplify the prior authorization process without requiring dramatic changes to provider behavior and payer. Web not a navinet user?
Locate The Proper Prior Authorization.
To get to anew tab. Web this authorization form will enable the third party listed above access to all present and future health plans available to your provider organization within navinet. All required fields (*) must be completed. Web providers need to request prior authorization for planned admissions of all ghp members, including geisinger gold (medicare advantage) and ghp family (managed medicaid).