Ingenio Rx Prior Authorization Form
Ingenio Rx Prior Authorization Form - We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. The form contains important information regarding the patient’s medical history and requested medication which anthem will use to determine whether or not the. The online process is faster and easier to complete, and the response is automatic, which helps patients get their medications sooner. Web prior (rx) authorization forms. Web members and providers can submit a pa for approval before a prescription is sent to a pharmacy. An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. Web our electronic prior authorization (epa) process is the preferred method for submitting pharmacy prior authorization requests. Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing. Improved electronic prior authorization process: If approved, the pharmacy claim then pays without interruption.
If approved, the pharmacy claim then pays without interruption. The food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory tract disease (lrtd) caused by respiratory syncytial virus (rsv) in individuals 60 years of age and older. We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. The online process is faster and easier to complete, and the response is automatic, which helps patients get their medications sooner. Web our electronic prior authorization (epa) process is the preferred method for submitting pharmacy prior authorization requests. The carelonrx name and carelonrx logo are registered trademarks. The form contains important information regarding the patient’s medical history and requested medication which anthem will use to determine whether or not the. Services provided by carelonrx, inc. Web updated june 02, 2022. An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost.
An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. Improved electronic prior authorization process: If approved, the pharmacy claim then pays without interruption. The carelonrx name and carelonrx logo are registered trademarks. The online process is faster and easier to complete, and the response is automatic, which helps patients get their medications sooner. Web updated june 02, 2022. The form contains important information regarding the patient’s medical history and requested medication which anthem will use to determine whether or not the. The food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory tract disease (lrtd) caused by respiratory syncytial virus (rsv) in individuals 60 years of age and older. Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing. Web improved electronic prior authorization process:
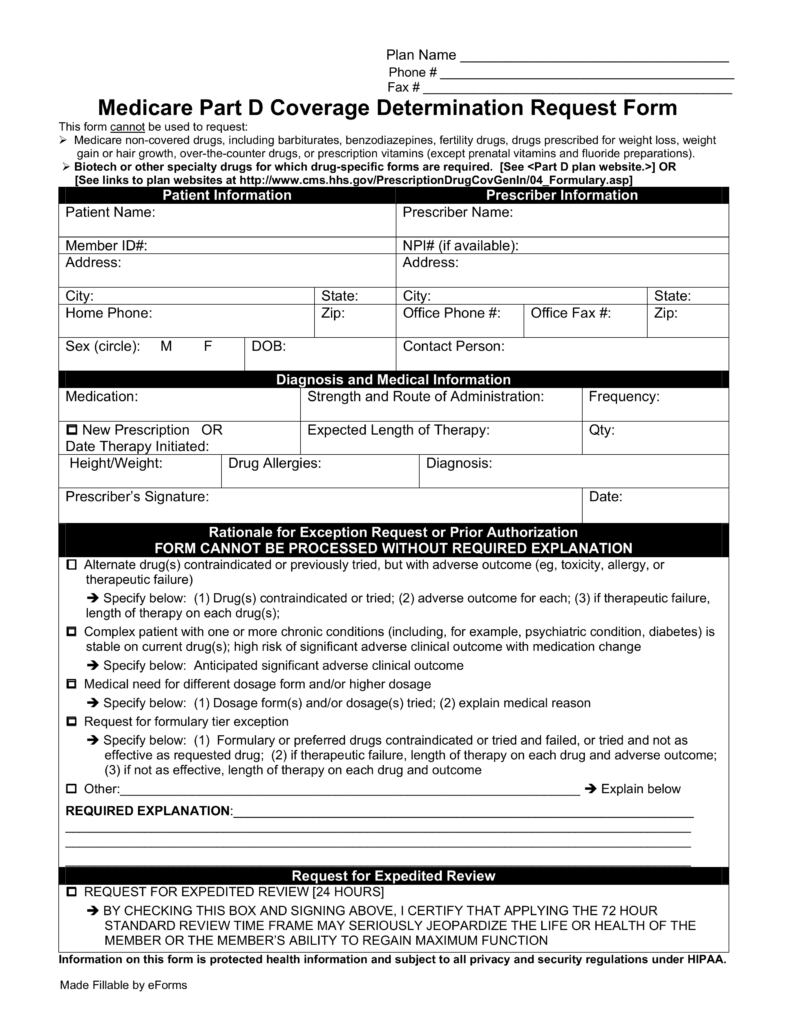
Free Medicare Prior (Rx) Authorization Form PDF eForms
Web prior (rx) authorization forms. Web improved electronic prior authorization process: We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. Web updated june 02, 2022. Improved electronic prior authorization process:
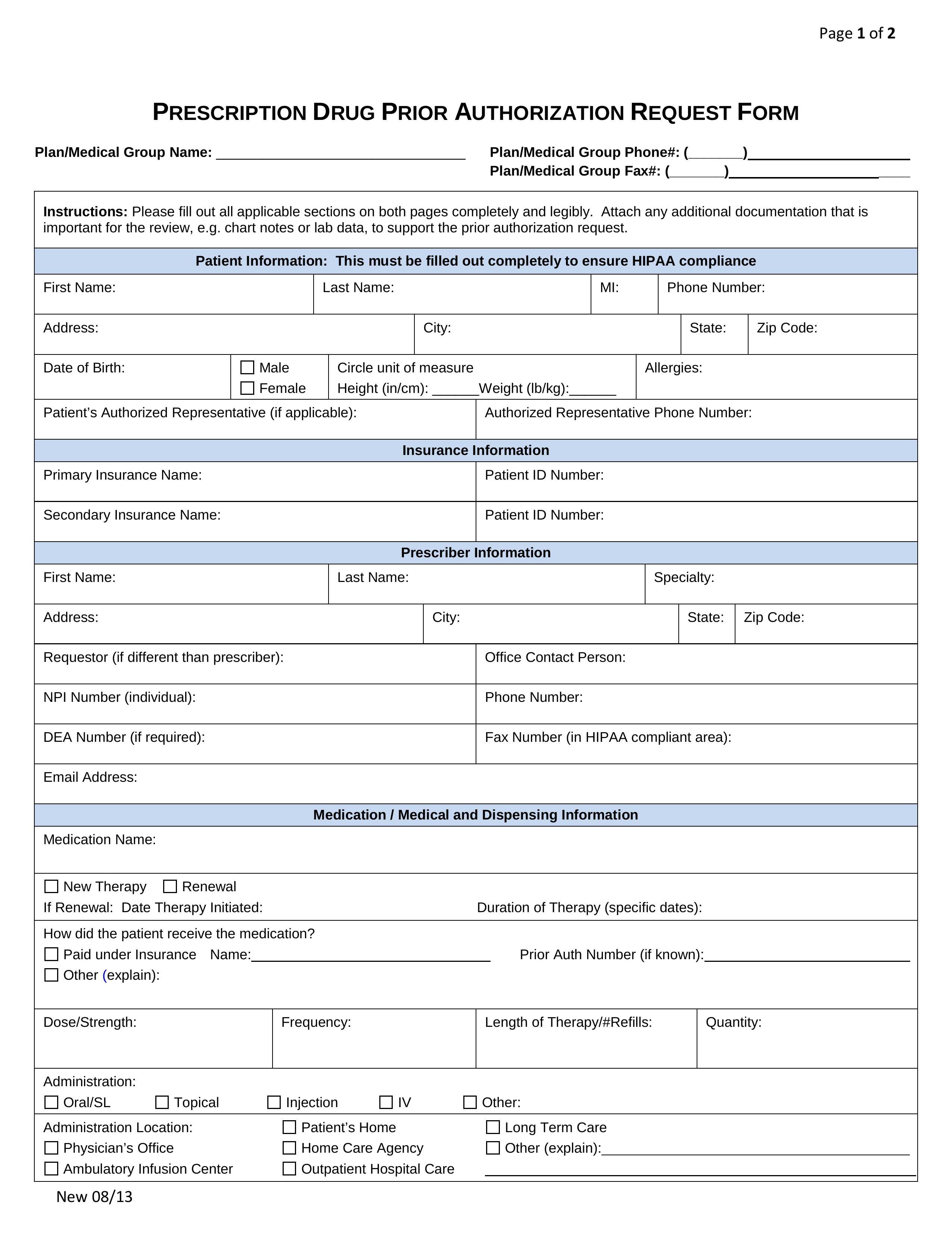
Free Prior (Rx) Authorization Forms PDF eForms
Web our electronic prior authorization (epa) process is the preferred method for submitting pharmacy prior authorization requests. Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing. Web improved electronic prior authorization process: Electronic pas (epas), which integrate with electronic medical record data, are the fastest way to submit and receive pa reviews.
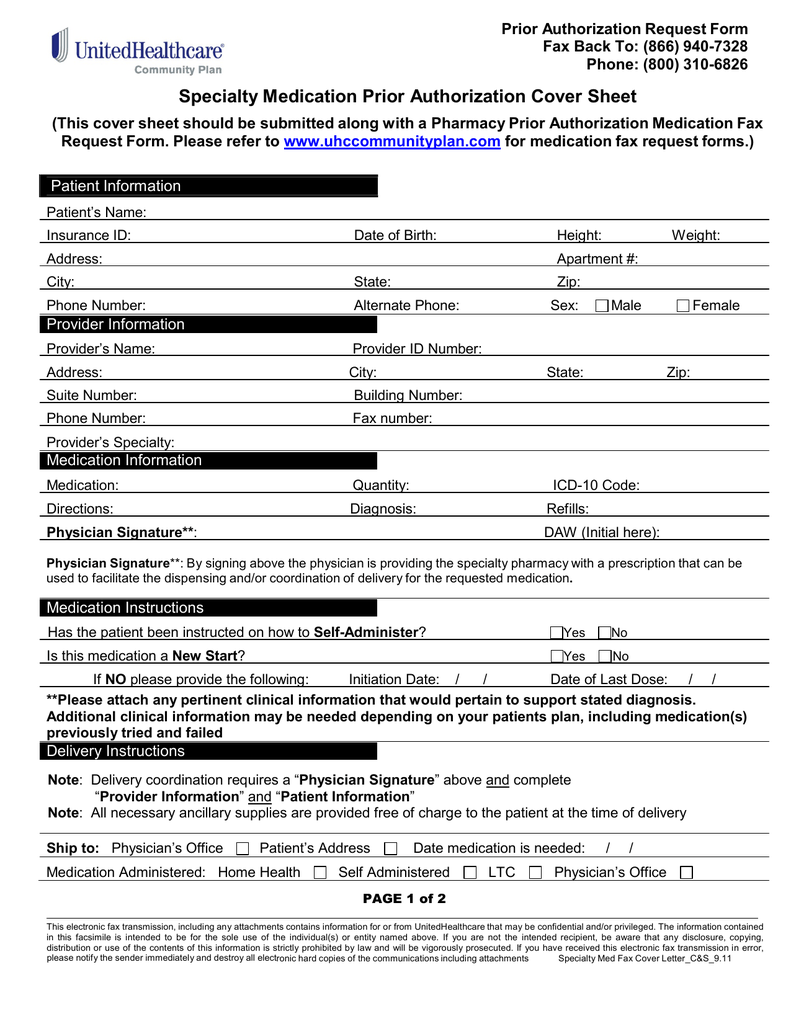
Specialty Medication Prior Authorization Cover Sheet
We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. The food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory tract disease (lrtd) caused by respiratory syncytial virus (rsv) in individuals 60 years of age and older. Web updated.
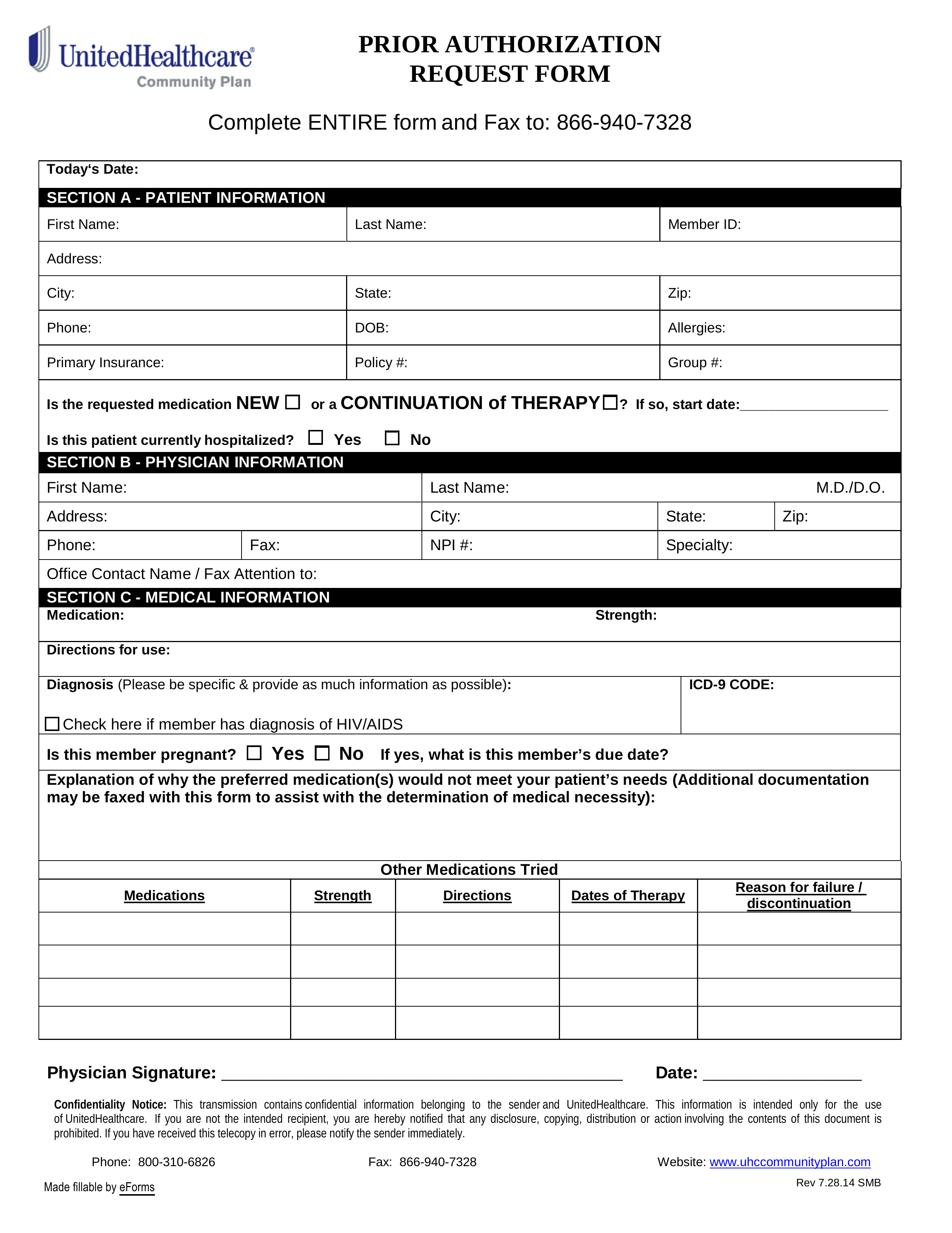
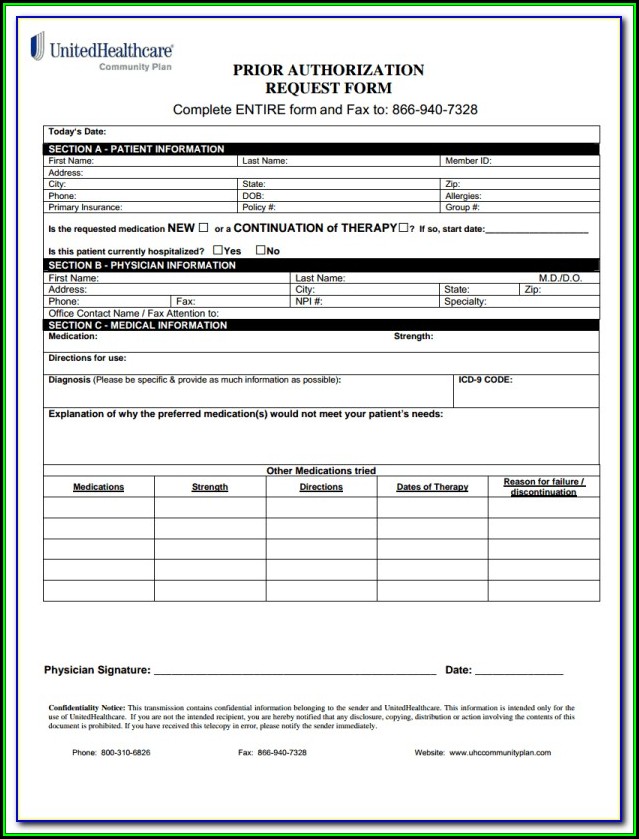
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
Web members and providers can submit a pa for approval before a prescription is sent to a pharmacy. Web our electronic prior authorization (epa) process is the preferred method for submitting pharmacy prior authorization requests. Web prior (rx) authorization forms. The food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory.
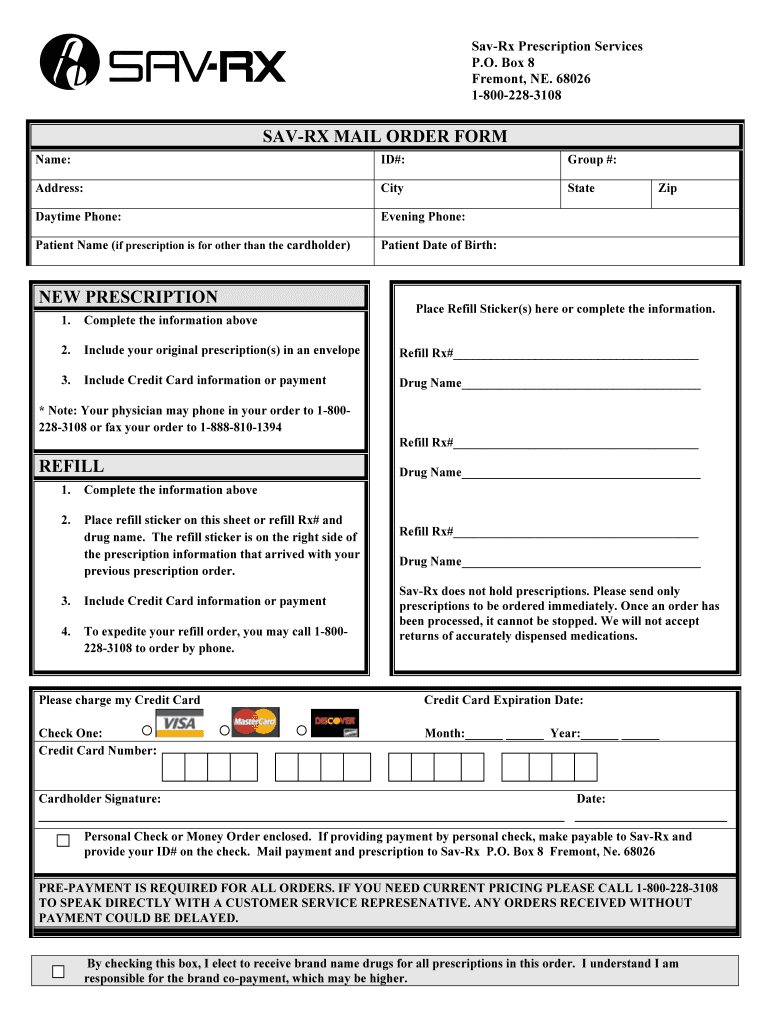
SavRx Mail Order Form Fill and Sign Printable Template Online US
Web improved electronic prior authorization process: Electronic pas (epas), which integrate with electronic medical record data, are the fastest way to submit and receive pa reviews and determinations. The online process is faster and easier to complete, and the response is automatic, which helps patients get their medications sooner. Web our electronic prior authorization (epa) process is the preferred method.
Optumrx Prior Authorization Form Cialis Rx Prior Authorization
Web updated june 02, 2022. Improved electronic prior authorization process: An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. If approved, the pharmacy claim then pays without interruption. Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing.
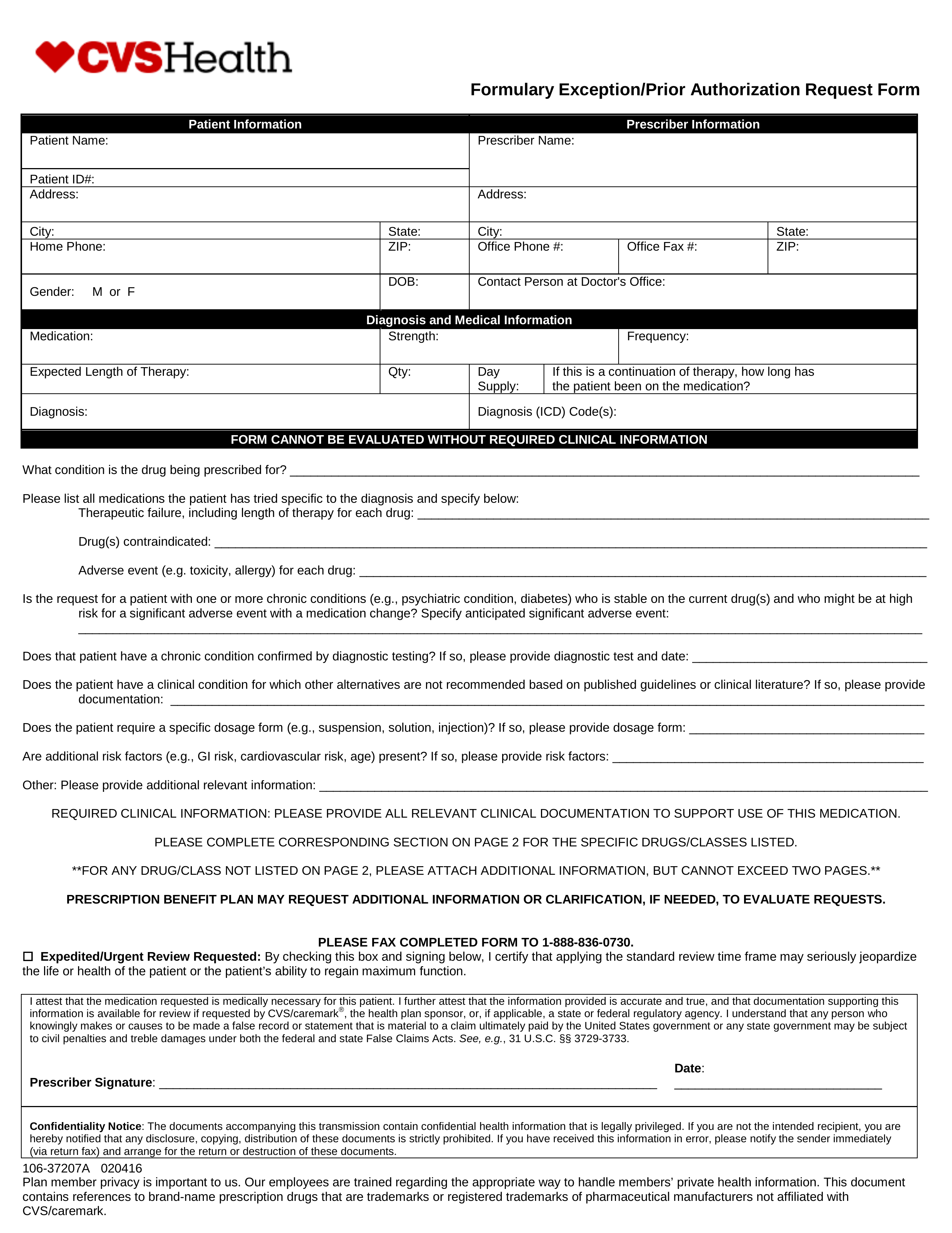
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
Web prior (rx) authorization forms. Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing. The online process is faster and easier to complete, and the response is automatic, which helps patients get their medications sooner. Services provided by carelonrx, inc. We’ve provided the following resources to help you understand anthem’s prior authorization.
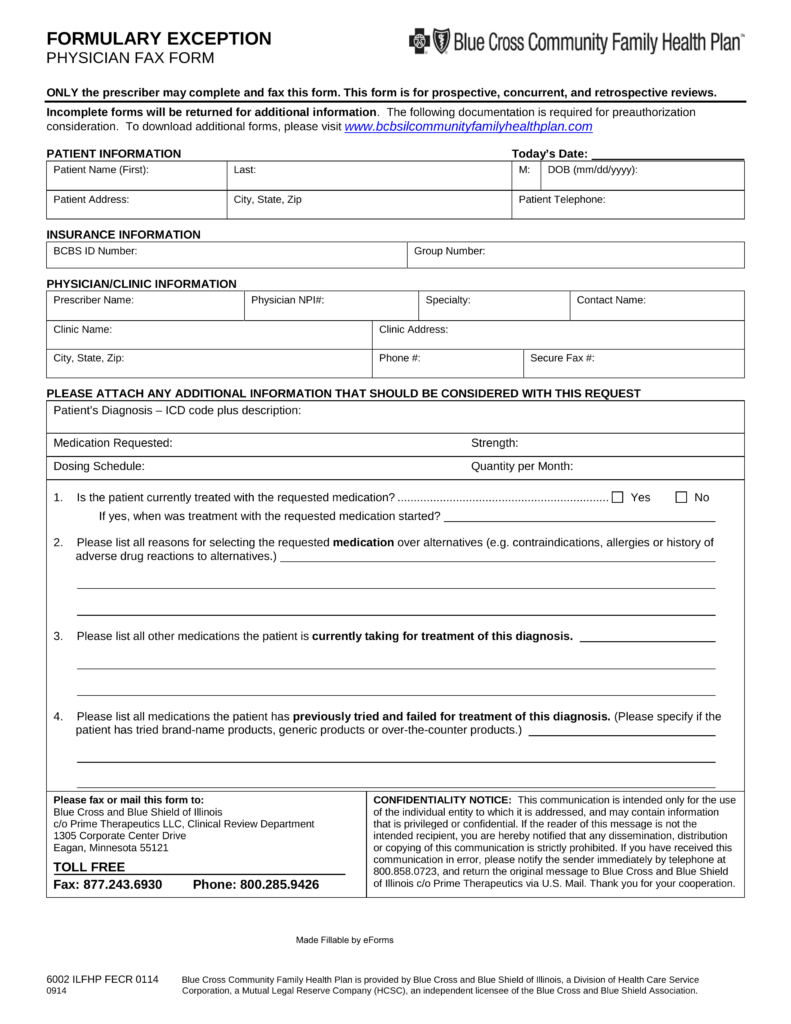
Free Prime Therapeutics Prior (Rx) Authorization Form PDF eForms
Web our electronic prior authorization (epa) process is the preferred method for submitting pharmacy prior authorization requests. Web prior (rx) authorization forms. If approved, the pharmacy claim then pays without interruption. Improved electronic prior authorization process: Web updated june 02, 2022.
Citizen Rx Prior Authorization form Beautiful Pdf Training Of
Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing. The carelonrx name and carelonrx logo are registered trademarks. Electronic pas (epas), which integrate with electronic medical record data, are the fastest way to submit and receive pa reviews and determinations. Web updated june 02, 2022. Electronic pas (epas), which integrate with electronic.
Prescription solutions Medicare Part D Prior Auth form Inspirational
Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing. The carelonrx name and carelonrx logo are registered trademarks. The food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory tract disease (lrtd) caused by respiratory syncytial virus (rsv) in individuals 60 years of.
Web Updated June 02, 2022.
The form contains important information regarding the patient’s medical history and requested medication which anthem will use to determine whether or not the. If approved, the pharmacy claim then pays without interruption. The food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory tract disease (lrtd) caused by respiratory syncytial virus (rsv) in individuals 60 years of age and older. Electronic pas (epas), which integrate with electronic medical record data, are the fastest way to submit and receive pa reviews and determinations.
Electronic Pas (Epas), Which Integrate With Electronic Medical Record Data, Are The Fastest Way To Submit And Receive Pa Reviews And.
Web improved electronic prior authorization process: Improved electronic prior authorization process: An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. Web prior (rx) authorization forms.
The Carelonrx Name And Carelonrx Logo Are Registered Trademarks.
Services provided by carelonrx, inc. Web members and providers can submit a pa for approval before a prescription is sent to a pharmacy. We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. Web we support doctors and pharmacists at every step, including digital resources for prior authorization and prescribing.
The Online Process Is Faster And Easier To Complete, And The Response Is Automatic, Which Helps Patients Get Their Medications Sooner.
Web our electronic prior authorization (epa) process is the preferred method for submitting pharmacy prior authorization requests.