Highmark Prior Authorization Form
Highmark Prior Authorization Form - Request for prescription medication for hospice, hospice prior authorization request form pdf. Extended release opioid prior authorization form. Authorization is based on medical necessity. Web home health the ordering provider is typically responsible for obtaining authorizations for the procedures/services included on the list of procedures/dme requiring authorization. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. This is called prior authorization. Member information member name member id date of birth diagnosis icd. Cymbalta, lyrica, savella) † testosterone therapies † miscellaneous items: Web use this form for all physical, occupational, speech, and feeding therapies, pulmonary and cardiac rehabilitation, and chiropractic care. To access all of the features on the highmark plan app, you must have active highmark medical coverage.
Diabetic testing supply request form. Web use this form for all physical, occupational, speech, and feeding therapies, pulmonary and cardiac rehabilitation, and chiropractic care. Web use this form to request coverage/prior authorization of medications for individuals in hospice care. The procedure codes contained on the list requiring authorization and related effective dates are subject to change. To access all of the features on the highmark plan app, you must have active highmark medical coverage. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Extended release opioid prior authorization form. Chronic inflammatory diseases medication request form. Review medication information and download pharmacy prior authorization forms. Designation of authorized representative form.
Extended release opioid prior authorization form. Extended release opioid prior authorization form. Cgrp inhibitors medication request form. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication request form diabetic testing supply request form dificid prior authorization form dupixent prior authorization form Web review and download prior authorization forms. In some cases, your prescription may not get covered. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Web how to request prior authorization/notification. Web pharmacy prior authorization forms. To access all of the features on the highmark plan app, you must have active highmark medical coverage.
FREE 10+ Sample Medicare Forms in PDF MS Word
To access all of the features on the highmark plan app, you must have active highmark medical coverage. Inpatient and outpatient authorization request form. When this happens, a prior authorization form is sent in for review. Web blood disorders medication request form. Web get the highmark plan app.
About Privacy Policy Copyright TOS Contact Sitemap
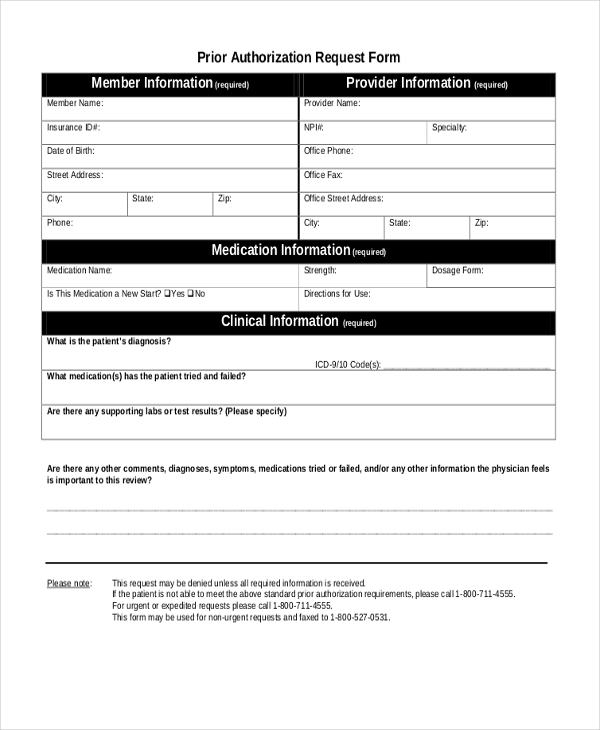
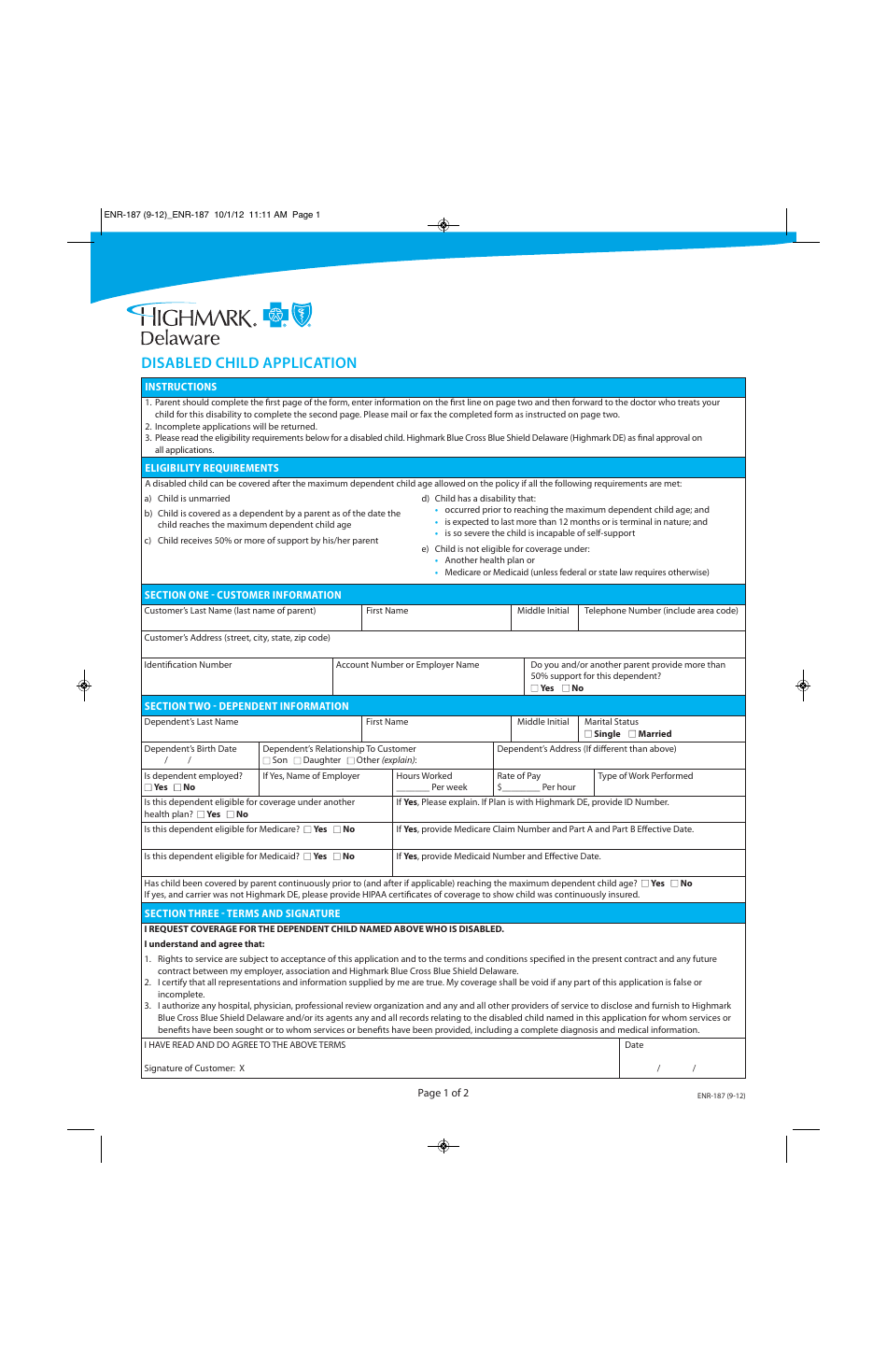
A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. Designation of personal representative for appeal process. The authorization is typically obtained by the ordering provider. Incomplete information or illegible forms will delay processing. Member information member name member id date of birth diagnosis icd.
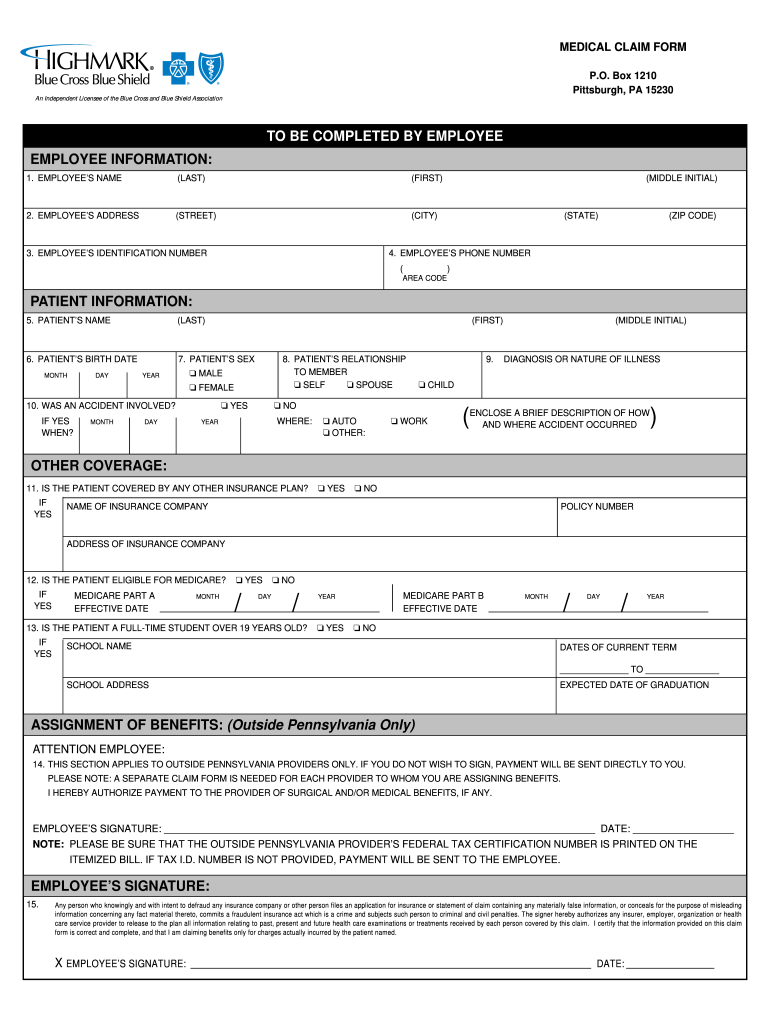
Highmark Claim Form Fill Out and Sign Printable PDF Template signNow
Web pharmacy prior authorization forms. Cymbalta, lyrica, savella) † testosterone therapies † miscellaneous items: Web get the highmark plan app. Using navinet is the preferred way to request prior authorization/notification from nia. Blood disorders medication request form.
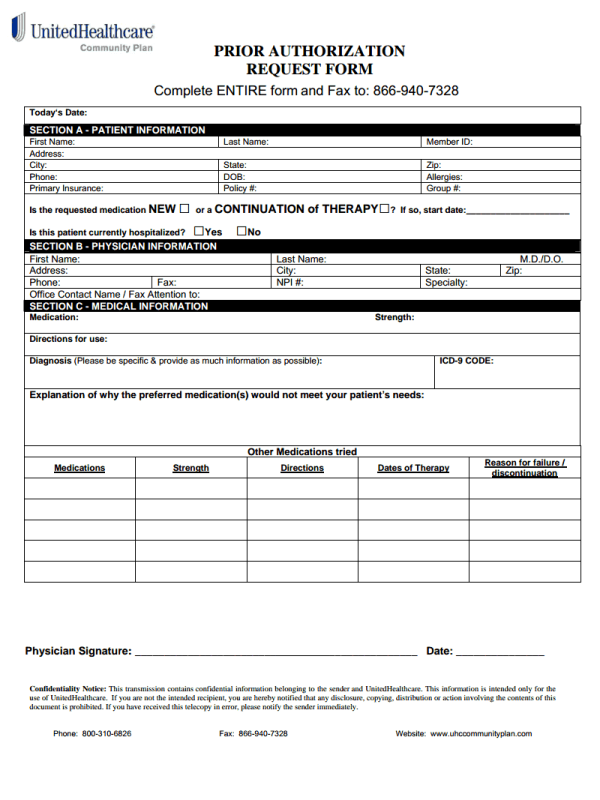
Simple UHC Prior Authorization Form for Everyone
To access all of the features on the highmark plan app, you must have active highmark medical coverage. Blood disorders medication request form. The procedure codes contained on the list requiring authorization and related effective dates are subject to change. In some cases, your prescription may not get covered. Extended release opioid prior authorization form.
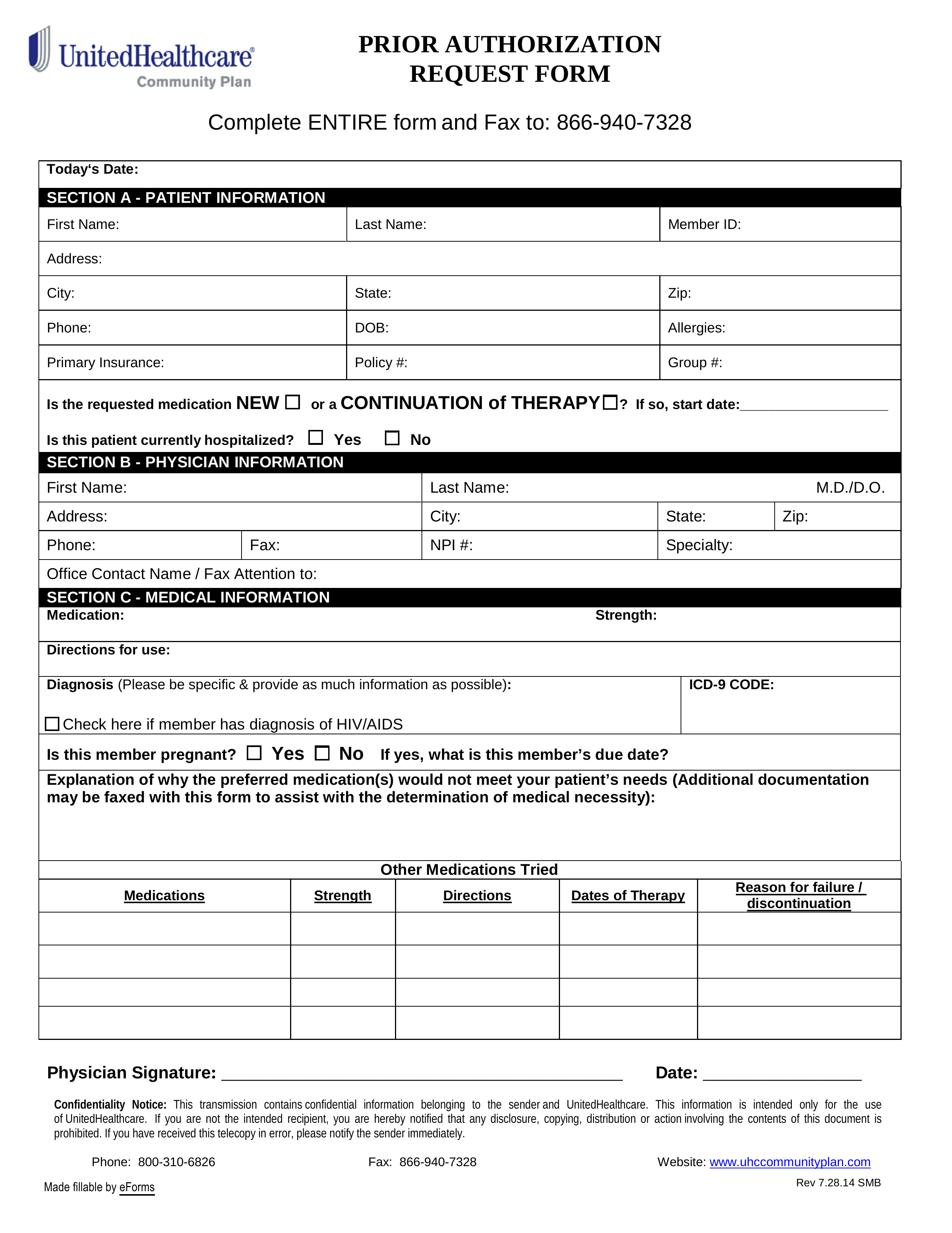
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
Cymbalta, lyrica, savella) † testosterone therapies † miscellaneous items: Chronic inflammatory diseases medication request form. Request for prescription medication for hospice, hospice prior authorization request form pdf. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Authorization is based on medical necessity.
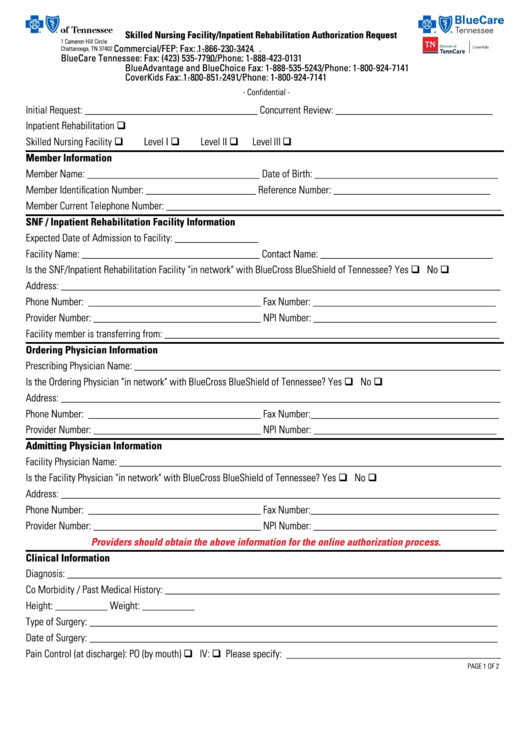
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
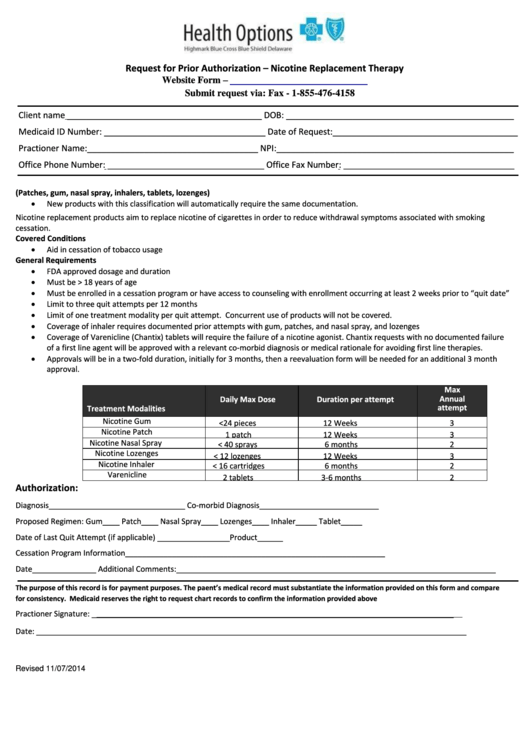
Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Web use this form to request coverage/prior authorization of medications for individuals in hospice care. Cymbalta, lyrica, savella) † testosterone.
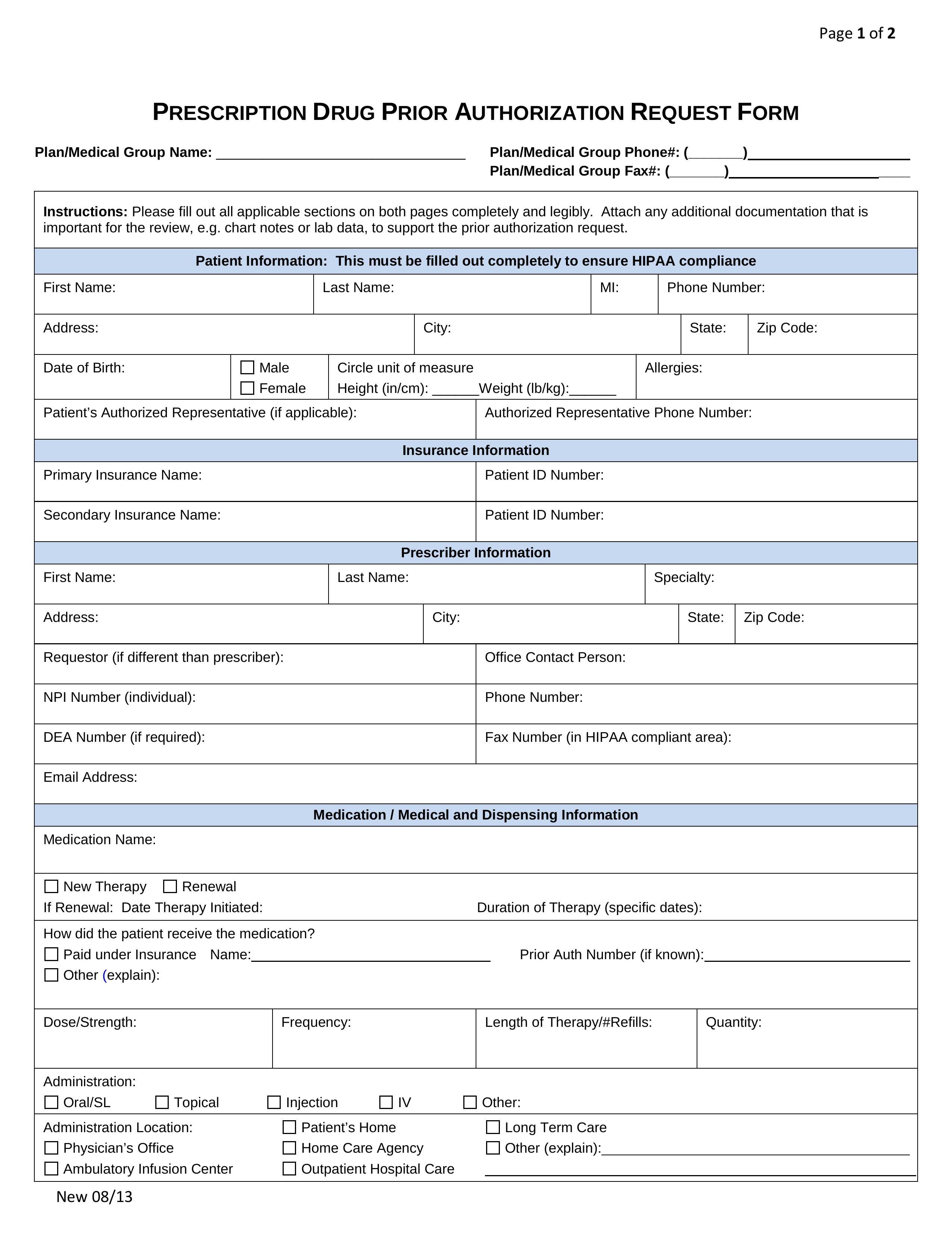
Free Prior (Rx) Authorization Forms PDF eForms
Medicare part d hospice prior authorization information. General provider forms & references after hours services betterdoctor provider faq certification for. To access all of the features on the highmark plan app, you must have active highmark medical coverage. Incomplete information or illegible forms will delay processing. When this happens, a prior authorization form is sent in for review.
Request For Prior Authorization Form Highmark Blue Cross Blue Shield
A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. In some cases, your prescription may not get covered. Diabetic testing supply request form. Chronic inflammatory diseases medication request form. The procedure codes contained on the list requiring authorization and related effective dates are subject to change.
Free Highmark Prior (Rx) Authorization Form PDF eForms
General provider forms & references after hours services betterdoctor provider faq certification for. Authorization is based on medical necessity. Inpatient and outpatient authorization request form. Web pharmacy prior authorization forms. Web prior authorization form please complete and fax all requested information below including any progress notes, laboratory test results, or chart documentation as applicable to pharmacy services.
Form ENR187 Download Printable PDF or Fill Online Disabled Child
Web requiring authorization pharmacy policy search miscellaneous forms on this page, you will find some recommended forms that providers may use when communicating with highmark, its members or other providers in the network. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. Web pharmacy prior authorization.
Authorization Is Based On Medical Necessity.
Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Chronic inflammatory diseases medication request form. Incomplete information or illegible forms will delay processing. Inpatient and outpatient authorization request form.
Designation Of Personal Representative For Appeal Process.
Review medication information and download pharmacy prior authorization forms. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement ofspecialists are required, plus additional information as specified: Web review and download prior authorization forms. Web use this form for all physical, occupational, speech, and feeding therapies, pulmonary and cardiac rehabilitation, and chiropractic care.
† Agents Used For Fibromyalgia (E.g.
Member information member name member id date of birth diagnosis icd. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Assignment of major medical claim form authorization for behavioral health providers to release. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization:
Web Get The Highmark Plan App.
In some cases, your prescription may not get covered. Web prior authorization form please complete and fax all requested information below including any progress notes, laboratory test results, or chart documentation as applicable to pharmacy services. Cgrp inhibitors medication request form. — your plan benefits are right there in the palm of your hand.