Highmark Blue Cross Blue Shield Prior Authorization Form
Highmark Blue Cross Blue Shield Prior Authorization Form - Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Brunory, janet (doi) created date: Some authorization requirements vary by member contract. Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29. Durable medical equipment over $500. Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Web updated june 02, 2022. Inpatient and outpatient authorization request form. Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. All inpatient admissions, including organ transplants.
Select the appropriate highmark blue shield form to get started. Web highmark blue shield has partnered with covermymeds to offer electronic prior authorization (epa) services. Inpatient and outpatient authorization request form. The authorization is typically obtained by the ordering provider. Any service that requires an authorization from a primary payer, except nonexhausted original medicare services. Some authorization requirements vary by member contract. Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52 76168de0730001 my blue access ppo premier gold 0 21 $ 471.19 $ 482.97. Web prior authorizations are required for: Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified:
Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified: Durable medical equipment over $500. Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. All inpatient admissions, including organ transplants. Brunory, janet (doi) created date: A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Web highmark blue shield has partnered with covermymeds to offer electronic prior authorization (epa) services.
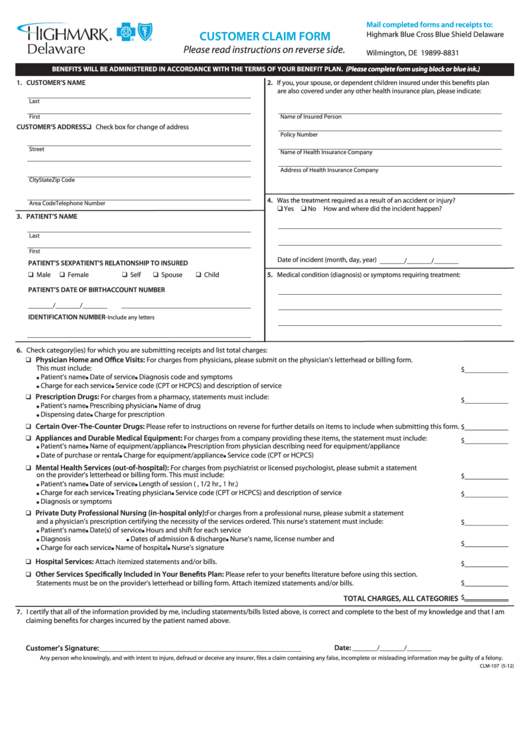
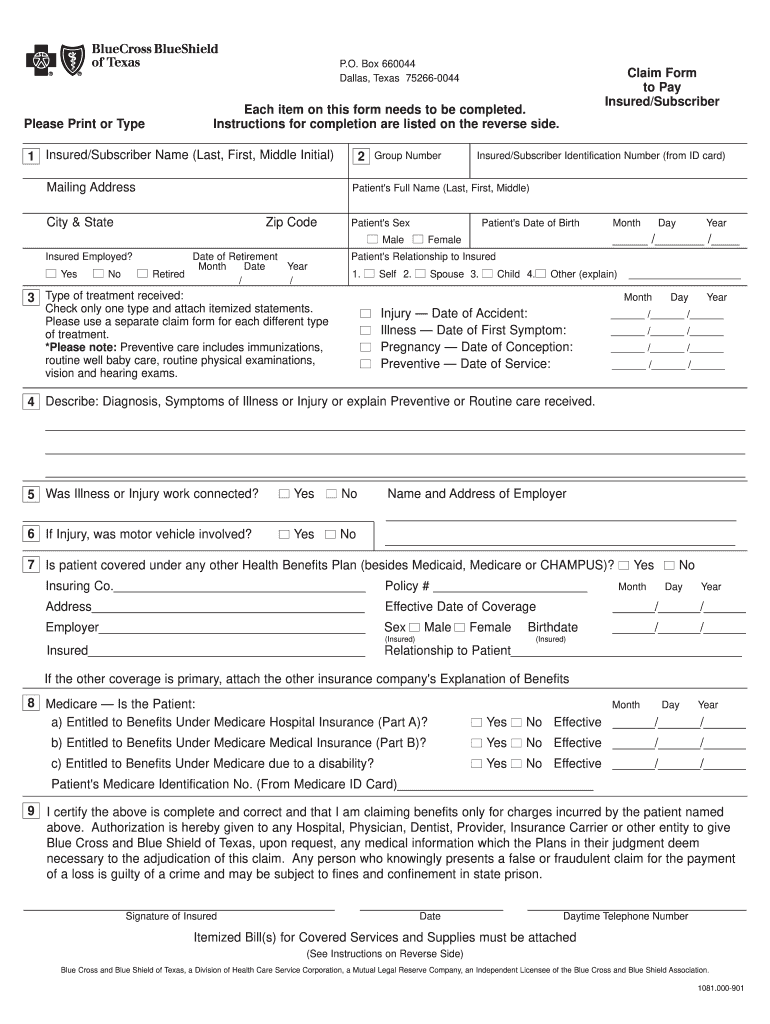
Customer Claim Form Highmark Blue Cross Blue Shield Delaware
Inpatient and outpatient authorization request form. Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29. Designation of authorized representative form. Select the appropriate highmark blue shield form to get started..
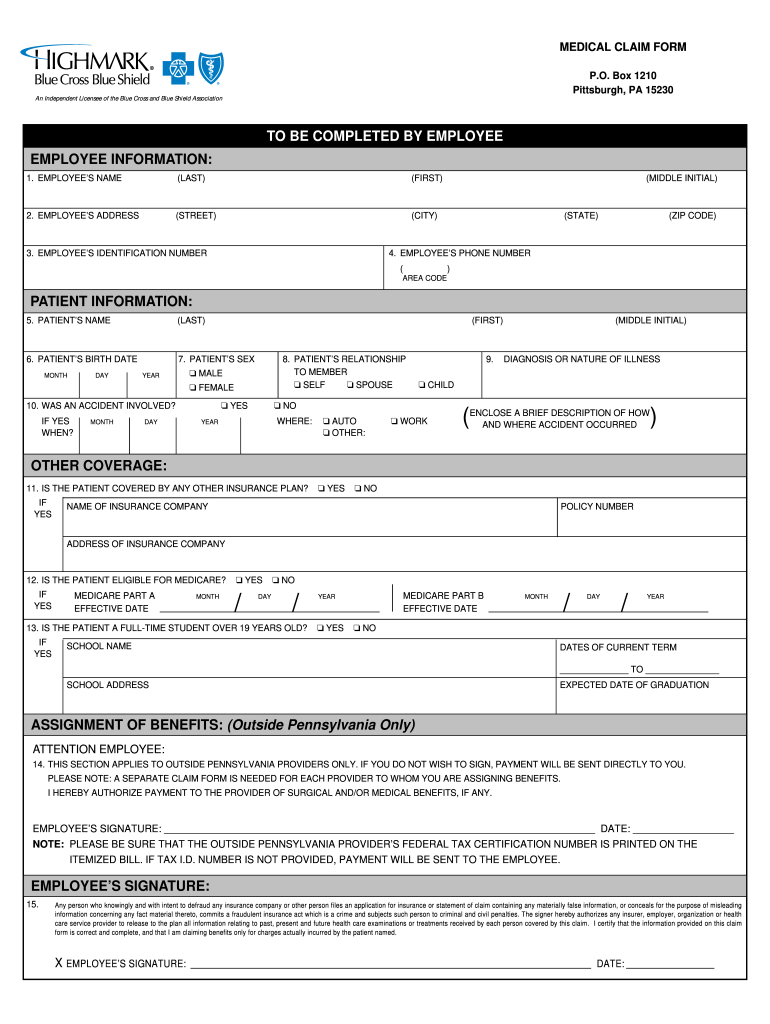
Highmark blue cross blue shield submit claim
The authorization is typically obtained by the ordering provider. Select the appropriate highmark blue shield form to get started. Web highmark blue shield has partnered with covermymeds to offer electronic prior authorization (epa) services. Brunory, janet (doi) created date: Durable medical equipment over $500.
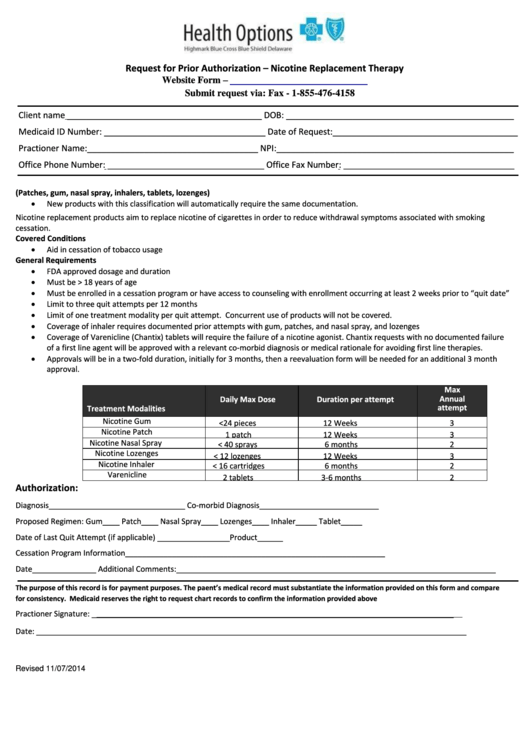
Request For Prior Authorization Form Highmark Blue Cross Blue Shield
Durable medical equipment over $500. Web updated june 02, 2022. Some authorization requirements vary by member contract. Inpatient and outpatient authorization request form. All inpatient admissions, including organ transplants.
ASC Coding and Billing Fundamentals Objectives PDF
A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Web highmark blue shield has partnered with covermymeds to offer electronic prior authorization (epa) services. Web prior authorizations are required for: Web updated june 02, 2022. Web prior authorization for the following drugs and/or therapeutic.
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Web updated june 02, 2022. Web.
Blue cross blue shield pennsylvania highmark availity
The authorization is typically obtained by the ordering provider. Select the appropriate highmark blue shield form to get started. Durable medical equipment over $500. Some authorization requirements vary by member contract. Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52 76168de0730001 my blue access ppo premier gold 0 21.
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Web updated june 02, 2022. The authorization is typically obtained by the ordering provider. Brunory, janet (doi) created date: Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests.
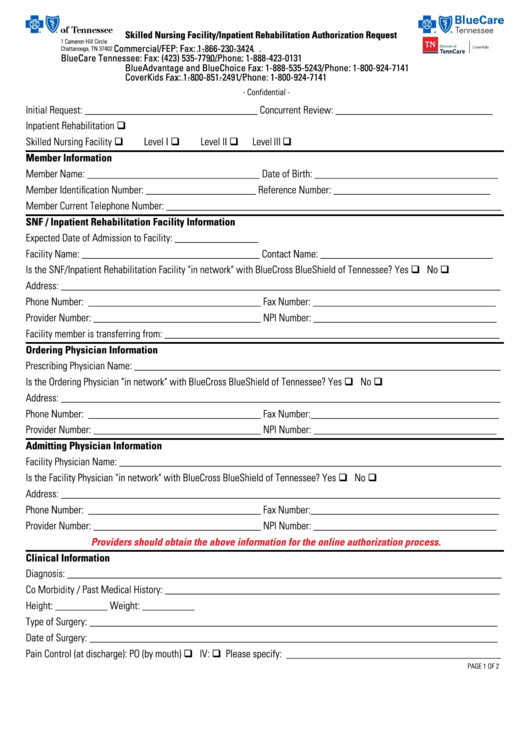
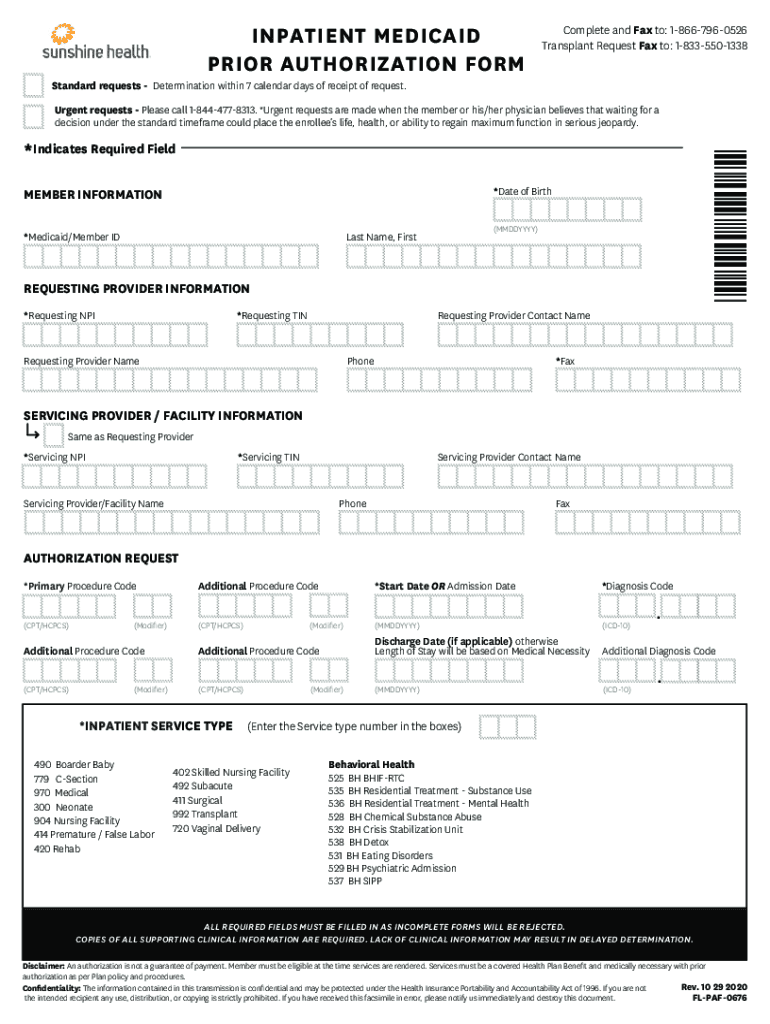
Priority Health Inpatient Authorization Form Fill Out and Sign
Any service that requires an authorization from a primary payer, except nonexhausted original medicare services. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Web 76168de0720001 my blue access.
Bcbs Claim Form Fill Out and Sign Printable PDF Template signNow
Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52 76168de0730001 my blue access ppo premier gold 0 21 $ 471.19 $ 482.97. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. Highmark blue cross blue.
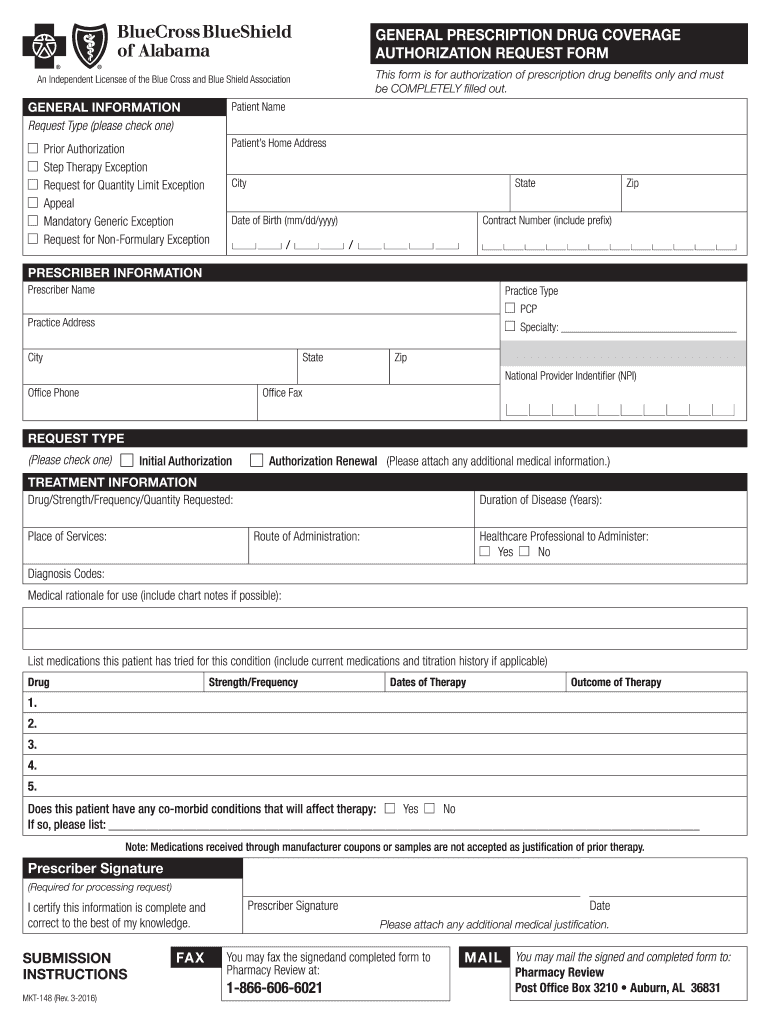
2008 Form AL BCBS MKT148 Fill Online, Printable, Fillable, Blank
Select the appropriate highmark blue shield form to get started. Any service that requires an authorization from a primary payer, except nonexhausted original medicare services. Inpatient and outpatient authorization request form. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral.
Web 76168De0720001 My Blue Access Major Events Ppo Catastrophic 9450 + 3 Free Pcp Visits 21 $ 274.65 $ 281.52 76168De0730001 My Blue Access Ppo Premier Gold 0 21 $ 471.19 $ 482.97.
Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29. Inpatient and outpatient authorization request form. Durable medical equipment over $500. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts.
A Highmark Prior Authorization Form Is A Document Used To Determine Whether A Patient’s Prescription Cost Will Be Covered By Their Highmark Health Insurance Plan.
Select the appropriate highmark blue shield form to get started. Any service that requires an authorization from a primary payer, except nonexhausted original medicare services. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified:
Highmark Blue Cross Blue Shield Delaware.
Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web highmark blue shield has partnered with covermymeds to offer electronic prior authorization (epa) services. Web prior authorizations are required for: Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service.
All Inpatient Admissions, Including Organ Transplants.
Web updated june 02, 2022. Some authorization requirements vary by member contract. Designation of authorized representative form. The authorization is typically obtained by the ordering provider.