Coordination Of Benefits Form
Coordination Of Benefits Form - Web coordination of benefits name of facility/provider patient name 1. The first or “primary payer” pays what it owes on your bills, and then sends the remainder of the bill Web cleveland clinic employee health plan coordination of benefits (cob) form coordination of benefits (cob) is the process used to pay healthcare insurance policy expenses when you or an eligible dependent is covered by more than one healthcare insurance policy, including medicare or medicaid. If yes, please complete all fields, sign and date. Please indicate the name of the carrier and effective date: Fill out this form if you and other members of your household are covered by more than one health insurance plan. See the coordination of benefits transactions basics. Web the coordination of benefits transaction is the transmission from any entity to a health plan for the purpose of determining the relative payment responsibilities of a health plan for health care claims or payment information. Id cards from all other health insurance plans full name and birth date for everyone covered by other insurance legal documents if anyone on your plan has other insurance because of a court order or divorce There are a variety of methods and programs used to identify situations in which medicare beneficiaries have other insurance that is primary to medicare.
Fill out this form if you and other members of your household are covered by more than one health insurance plan. Web “coordination of benefits.” if you have medicare and other health or drug coverage, each type of coverage is called a “payer.” when there’s more than one potential payer, there are coordination rules to decide who pays first. The plan that covers the individual as an employee will generally pay primary and the plan that covers the individual as a dependent will generally be the secondary payor. Type of other coverage 2. Network health will communicate with the other health insurance company to determine which company pays for each claim. See the coordination of benefits transactions basics. Do you or another family member have other health coverage that may cover this claim? Do you have other coverage through another group health plan? There are a variety of methods and programs used to identify situations in which medicare beneficiaries have other insurance that is primary to medicare. The bcrc does not process claims, nor does it handle any ghp related mistaken payment recoveries or claims specific inquiries.
Web coordination of benefits form. The bcrc does not process claims, nor does it handle any ghp related mistaken payment recoveries or claims specific inquiries. Web the bcrc takes actions to identify the health benefits available to a beneficiary and coordinates the payment process to prevent mistaken payment of medicare benefits. Please indicate the name of the carrier and effective date: Type of other coverage 2. Web coordination of benefits name of facility/provider patient name 1. If no, please provide the information within section one, sign and date. If so, are you covered as an active employee or a retiree? See the coordination of benefits transactions basics. Fill out this form if you and other members of your household are covered by more than one health insurance plan.
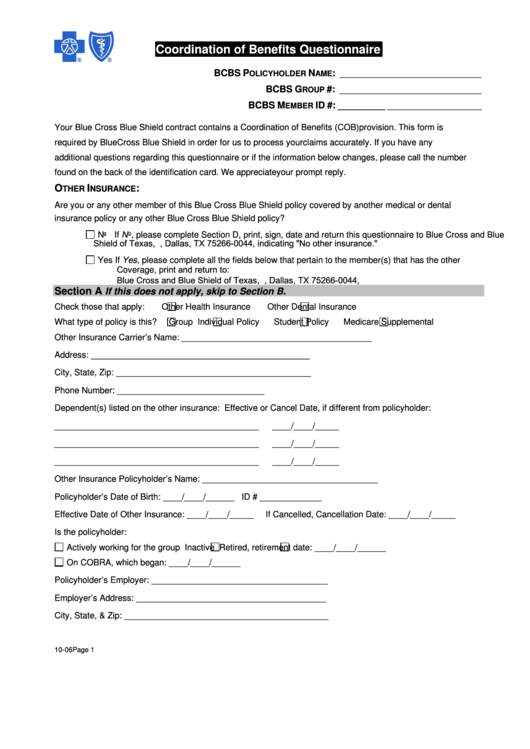
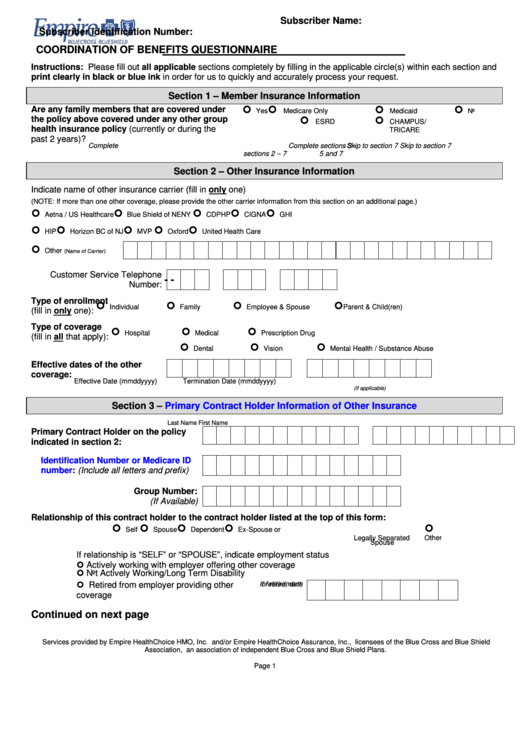
Fillable Bcbs Coordination Of Benefits Questionnaire printable pdf download
Do you have other coverage through another group health plan? The first or “primary payer” pays what it owes on your bills, and then sends the remainder of the bill Web before letting us know about coordination of benefits, you'll need to gather the following documents: The bcrc does not process claims, nor does it handle any ghp related mistaken.
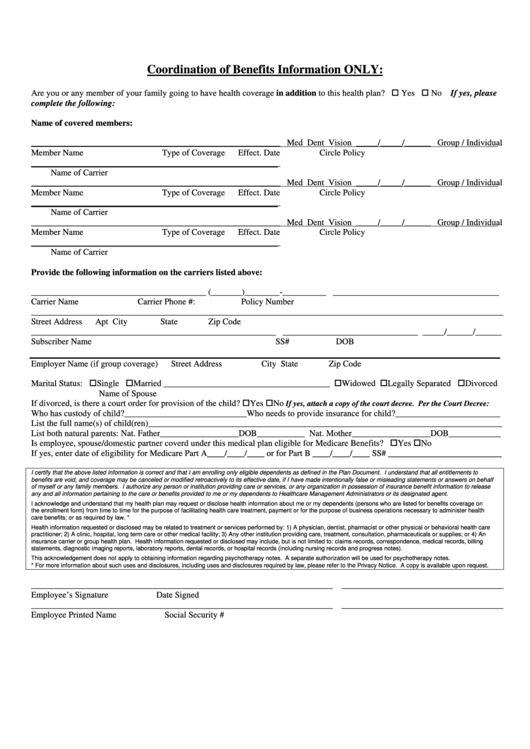
Coordination Of Benefits Information printable pdf download
Web the coordination of benefits transaction is the transmission from any entity to a health plan for the purpose of determining the relative payment responsibilities of a health plan for health care claims or payment information. Type of other coverage 2. Do you have other coverage through another group health plan? There are a variety of methods and programs used.
Understanding Coordination of Benefits Eligible Community
See the coordination of benefits transactions basics. Do you have other coverage through another group health plan? Fill out this form if you and other members of your household are covered by more than one health insurance plan. Type of other coverage 2. The bcrc does not process claims, nor does it handle any ghp related mistaken payment recoveries or.
Anthem Coordination Of Benefits Form Fill Online, Printable, Fillable
See the coordination of benefits transactions basics. Web coordination of benefits (cob) form section i 1. The plan that covers the individual as an employee will generally pay primary and the plan that covers the individual as a dependent will generally be the secondary payor. Web coordination of benefits name of facility/provider patient name 1. Web the coordination of benefits.
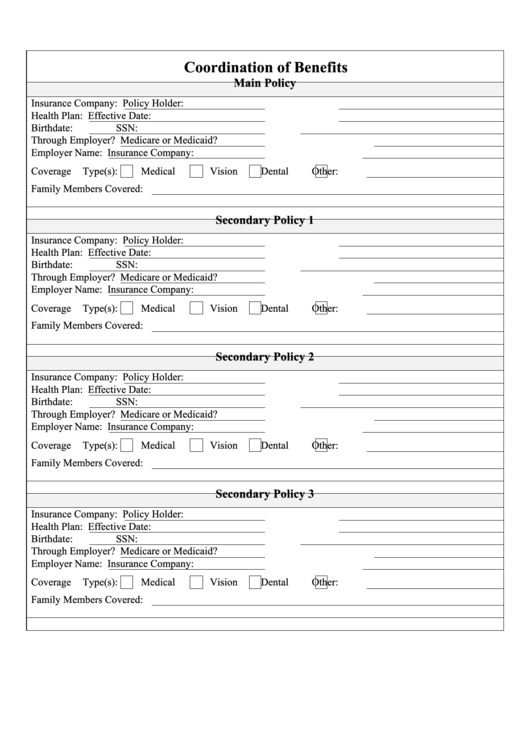
Coordination Of Benefits printable pdf download
Web coordination of benefits name of facility/provider patient name 1. Do you have other coverage through another group health plan? Web the coordination of benefits transaction is the transmission from any entity to a health plan for the purpose of determining the relative payment responsibilities of a health plan for health care claims or payment information. If so, are you.
Blockchain & Group Benefit Coordination Learnings & Wrap Up
Fill out this form if you and other members of your household are covered by more than one health insurance plan. See the coordination of benefits transactions basics. Web coordination of benefits name of facility/provider patient name 1. There are a variety of methods and programs used to identify situations in which medicare beneficiaries have other insurance that is primary.
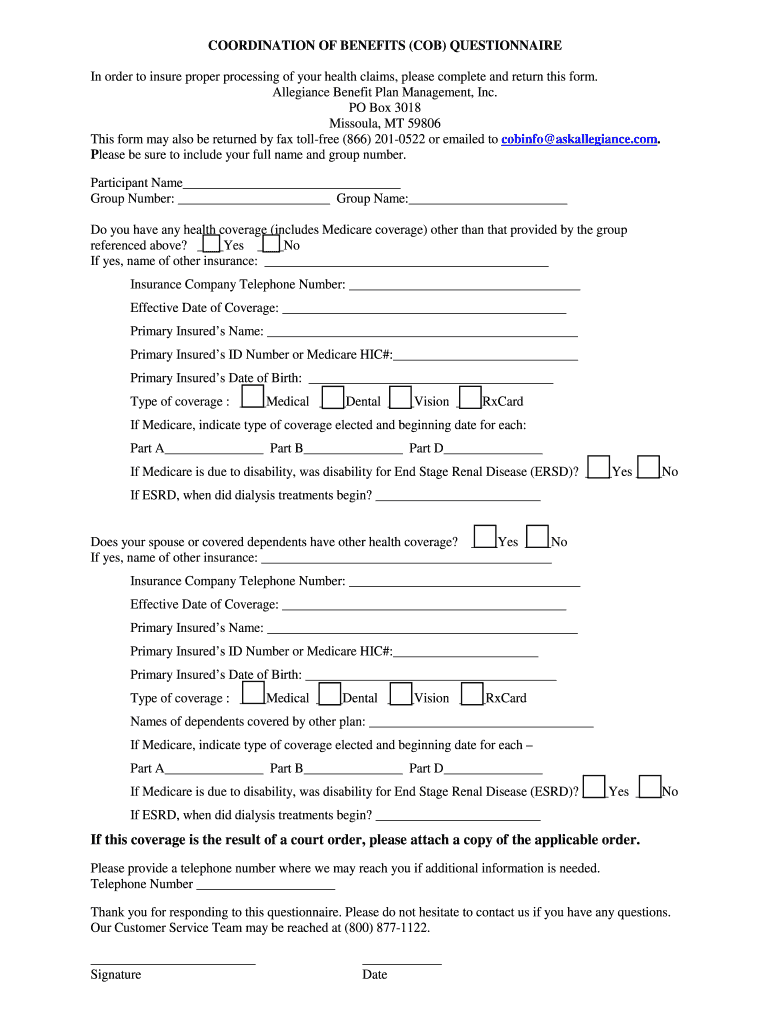
Benefits Cob Questionnaire Form Fill Out and Sign Printable PDF
Web the coordination of benefits transaction is the transmission from any entity to a health plan for the purpose of determining the relative payment responsibilities of a health plan for health care claims or payment information. Do you have other coverage through another group health plan? Id cards from all other health insurance plans full name and birth date for.
Coordination Of Benefits Questionnaire Empire Blue Cross Blue Shield
Please indicate the name of the carrier and effective date: Web coordination of benefits (cob) form section i 1. See the coordination of benefits transactions basics. Web the coordination of benefits transaction is the transmission from any entity to a health plan for the purpose of determining the relative payment responsibilities of a health plan for health care claims or.
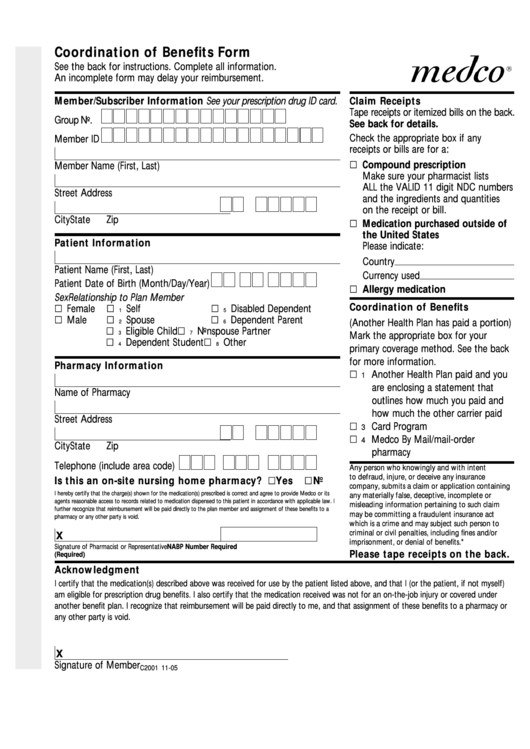
Form C2001 Coordination Of Benefits Form printable pdf download
If no, please provide the information within section one, sign and date. The plan that covers the individual as an employee will generally pay primary and the plan that covers the individual as a dependent will generally be the secondary payor. Type of other coverage 2. Web “coordination of benefits.” if you have medicare and other health or drug coverage,.
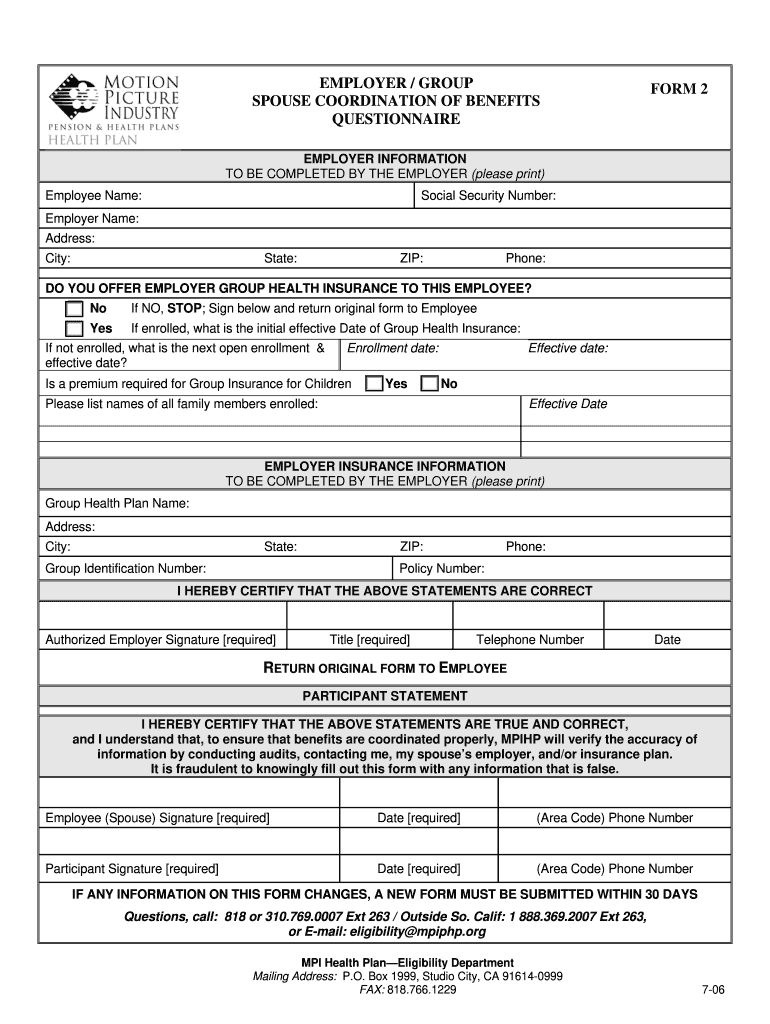
Mpiphp Forms Fill Out and Sign Printable PDF Template signNow
See the coordination of benefits transactions basics. The plan that covers the individual as an employee will generally pay primary and the plan that covers the individual as a dependent will generally be the secondary payor. Web before letting us know about coordination of benefits, you'll need to gather the following documents: Web the bcrc takes actions to identify the.
See The Coordination Of Benefits Transactions Basics.
Web the coordination of benefits transaction is the transmission from any entity to a health plan for the purpose of determining the relative payment responsibilities of a health plan for health care claims or payment information. Web the bcrc takes actions to identify the health benefits available to a beneficiary and coordinates the payment process to prevent mistaken payment of medicare benefits. Web cleveland clinic employee health plan coordination of benefits (cob) form coordination of benefits (cob) is the process used to pay healthcare insurance policy expenses when you or an eligible dependent is covered by more than one healthcare insurance policy, including medicare or medicaid. Web “coordination of benefits.” if you have medicare and other health or drug coverage, each type of coverage is called a “payer.” when there’s more than one potential payer, there are coordination rules to decide who pays first.
The First Or “Primary Payer” Pays What It Owes On Your Bills, And Then Sends The Remainder Of The Bill
Web most coordination of benefit provisions include the following general rules for employees and spouses covered by two group health plans: Web if a beneficiary has medicare and other health insurance, coordination of benefits (cob) rules decide which entity pays first. Please indicate the name of the carrier and effective date: The bcrc does not process claims, nor does it handle any ghp related mistaken payment recoveries or claims specific inquiries.
Do You Or Another Family Member Have Other Health Coverage That May Cover This Claim?
Do you have other coverage through another group health plan? Web before letting us know about coordination of benefits, you'll need to gather the following documents: Web coordination of benefits (cob) form section i 1. Type of other coverage 2.
If No, Please Provide The Information Within Section One, Sign And Date.
Network health will communicate with the other health insurance company to determine which company pays for each claim. Fill out this form if you and other members of your household are covered by more than one health insurance plan. There are a variety of methods and programs used to identify situations in which medicare beneficiaries have other insurance that is primary to medicare. The plan that covers the individual as an employee will generally pay primary and the plan that covers the individual as a dependent will generally be the secondary payor.