Ambetter Appeal Form Texas
Ambetter Appeal Form Texas - Web use this form as part of the ambetter from coordinated care request for reconsideration and claim dispute process. Ambetter from arizona complete health attn: Web a claim dispute/claim appeal must be submitted on this claim dispute/appeal form, which can also be found on our website. Select your state to contact an ambetter representative in your service area. Use your zip code to find your personal plan. The completed form can be returned by mail or fax. Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) grievance and appeals; Web fax authorization request primary procedure code* additional procedure code start date or admission date * diagnosis code * (cpt/hcpcs) (modifier). Web the panel will make a recommendation for the final decision on the member complaint, and ambetter’s final decision will be provided to the member within thirty (30) days of the. Web if you have questions or concerns about your health insurance coverage, we'd love to hear from you.
Biopharmacy outpatient prior authorization form (j. Complex imaging, mra, mri, pet, and ct scans, as well as speech, occupational and physical. Web appeal by phone, fax, or in person. Ambetter from arizona complete health attn: Easily fill out pdf blank, edit, and sign them. Read below to find out how to appeal a decision, file a complaint, and ask for an external. Provider disputes po box 9040. All fields are required information a request for. Web if you have questions or concerns about your health insurance coverage, we'd love to hear from you. You must file an appeal within 180 days of the date on the denial letter.
Web the procedures for filing a complaint/grievance or appeal are outlined in the ambetter member’s evidence of coverage. Web if you have questions or concerns about your health insurance coverage, we'd love to hear from you. Web a claim dispute/claim appeal must be submitted on this claim dispute/appeal form, which can also be found on our website. Web español if you disagree with a decision made by your health plan, you have several options. You must file an appeal within 180 days of the date on the denial letter. Biopharmacy outpatient prior authorization form (j. Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) grievance and appeals; Web forms claims claims appeal (pdf) claims reconsideration (pdf) cms1500 (pdf) corrected claim (pdf) request for claim status (pdf) ub04 (pdf) member. Web • ambetter will acknowledge receipt within 10 business days of receiving the appeal. See coverage in your area;
ambetter secure care 20 darlenaohlemacher
The claim dispute form must be completed in its. Web complete ambetter reconsideration form texas online with us legal forms. Web the procedures for filing a complaint/grievance or appeal are outlined in the ambetter member’s evidence of coverage. The completed form can be returned by mail or fax. • ambetter will resolve each appeal and provide written notice as expeditiously.
Ambetter Prior Authorization form Awesome Lookasserta Urlscan
Web complete ambetter reconsideration form texas online with us legal forms. Complex imaging, mra, mri, pet, and ct scans, as well as speech, occupational and physical. Web a claim dispute/claim appeal must be submitted on this claim dispute/appeal form, which can also be found on our website. Web you, your provider, a friend, a relative, lawyer or another spokesperson can.
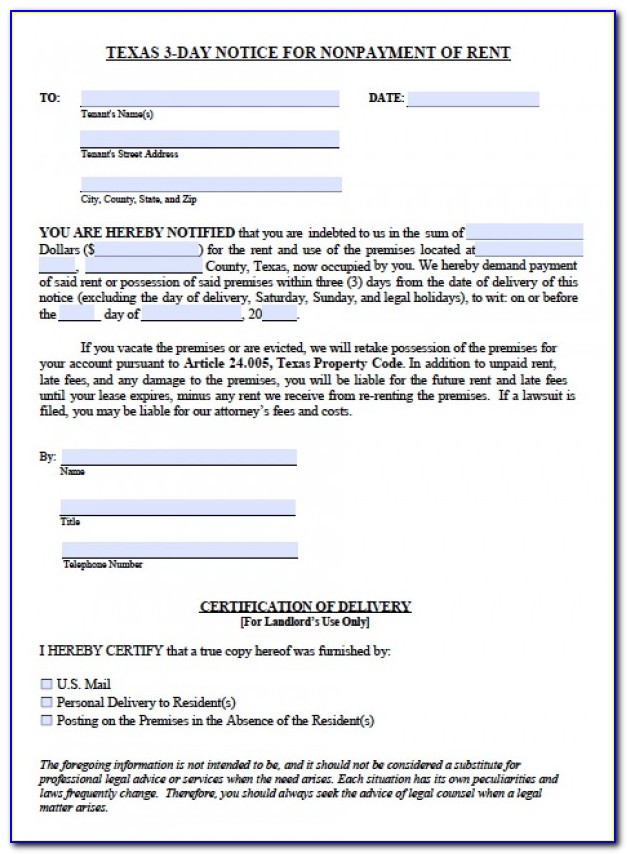
Texas Notice Of Appeal Form Fill Online, Printable, Fillable, Blank
See coverage in your area; Web forms claims claims appeal (pdf) claims reconsideration (pdf) cms1500 (pdf) corrected claim (pdf) request for claim status (pdf) ub04 (pdf) member. Easily fill out pdf blank, edit, and sign them. • ambetter will resolve each appeal and provide written notice as expeditiously as the. You must file an appeal within 180 days of the.
What Is The Group Id For Ambetter / Where can I find the policy number
Web forms claims claims appeal (pdf) claims reconsideration (pdf) cms1500 (pdf) corrected claim (pdf) request for claim status (pdf) ub04 (pdf) member. Web appeal you file an appeal in response to a denial received from ambetter from health net. Web español if you disagree with a decision made by your health plan, you have several options. Web you will need.
Ambetter Insurance Providers Texas / Ambetter From Coordinated Care
Web español if you disagree with a decision made by your health plan, you have several options. Use your zip code to find your personal plan. Web a claim dispute/claim appeal must be submitted on this claim dispute/appeal form, which can also be found on our website. Web fax authorization request primary procedure code* additional procedure code start date or.
Ambetter Prior Authorization form Brilliant Envision Rx Prior
Web appeal by phone, fax, or in person. Read below to find out how to appeal a decision, file a complaint, and ask for an external. Web a claim dispute/claim appeal must be submitted on this claim dispute/appeal form, which can also be found on our website. Web complete ambetter reconsideration form texas online with us legal forms. Web find.
Consumer Debt Litigation (mostly Texas) Appealing Pro Se in Texas
All fields are required information a request for. Web appeal by phone, fax, or in person. Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) grievance and appeals; Web if you have questions or concerns about your health insurance coverage, we'd love to hear from you. Web • ambetter will acknowledge receipt within 10 business days.
What Is The Group Id For Ambetter Ambetter Insurance Card Images
Web the panel will make a recommendation for the final decision on the member complaint, and ambetter’s final decision will be provided to the member within thirty (30) days of the. Web appeal by phone, fax, or in person. Web español if you disagree with a decision made by your health plan, you have several options. Web use this form.
Ambetter Insurance Texas Providers Ambetter Superior Health Plan
Biopharmacy outpatient prior authorization form (j. Web you, your provider, a friend, a relative, lawyer or another spokesperson can request an appeal and complete the appeal form on your behalf. Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) grievance and appeals; Web the procedures for filing a complaint/grievance or appeal are outlined in the ambetter.
3 Day Eviction Notice California Form
Easily fill out pdf blank, edit, and sign them. • ambetter will resolve each appeal and provide written notice as expeditiously as the. Access the find a provider guide, member handbook, and reimbursement forms. Web • ambetter will acknowledge receipt within 10 business days of receiving the appeal. Mail completed form(s) and attachments to the appropriate address:
Web Use This Form As Part Of The Ambetter From Coordinated Care Request For Reconsideration And Claim Dispute Process.
If you have questions about the. Easily fill out pdf blank, edit, and sign them. Ambetter from arizona complete health attn: Complex imaging, mra, mri, pet, and ct scans, as well as speech, occupational and physical.
Use Your Zip Code To Find Your Personal Plan.
Web the panel will make a recommendation for the final decision on the member complaint, and ambetter’s final decision will be provided to the member within thirty (30) days of the. Select your state to contact an ambetter representative in your service area. Access the find a provider guide, member handbook, and reimbursement forms. Web find our member handbooks, forms, and resources all in one place!
Mail Completed Form(S) And Attachments To The Appropriate Address:
You must file an appeal within 180 days of the date on the denial letter. All fields are required information a request for. This could be a denial of coverage for requested medical care or for a claim you filed for. Web a claim dispute/claim appeal must be submitted on this claim dispute/appeal form, which can also be found on our website.
• Ambetter Will Resolve Each Appeal And Provide Written Notice As Expeditiously As The.
Web appeal you file an appeal in response to a denial received from ambetter from health net. Biopharmacy outpatient prior authorization form (j. Provider disputes po box 9040. Web the procedures for filing a complaint/grievance or appeal are outlined in the ambetter member’s evidence of coverage.